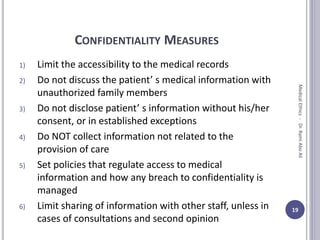
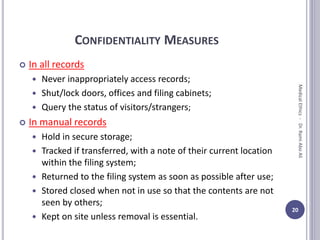
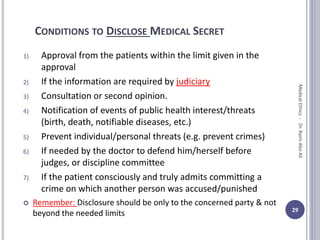
This document discusses medical ethics and legal medicine related to confidentiality and privacy. It begins by defining privacy and confidentiality, noting that privacy respects a patient's body while confidentiality respects their personal medical information. It then outlines various measures to protect patient privacy during medical examinations and treatments. The document also discusses the concept of medical secrets and the duty of confidentiality, the importance of which is enshrined in ethics codes and laws. Exceptions to maintaining confidentiality are noted, as well as measures to protect confidential information and ensure it is kept private.