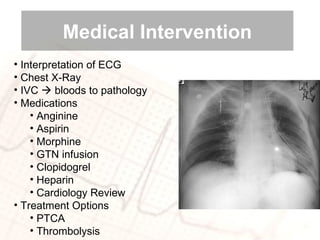
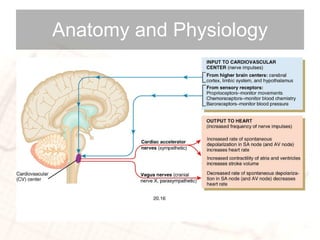
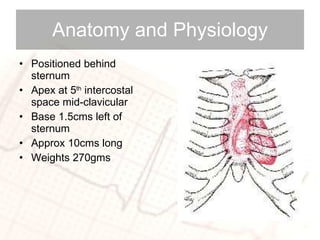
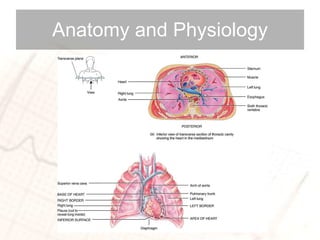
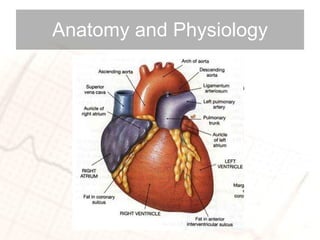
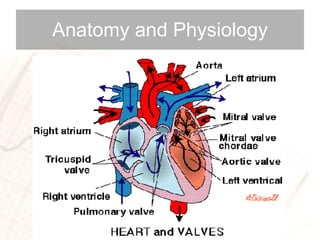
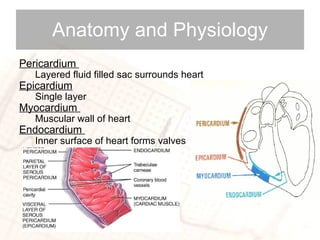
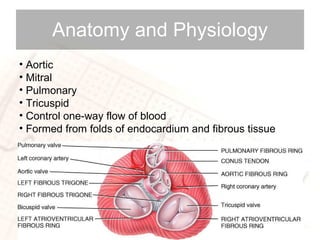
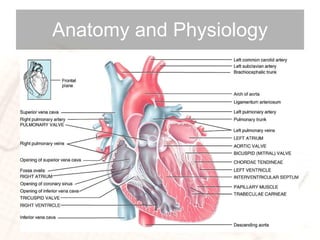
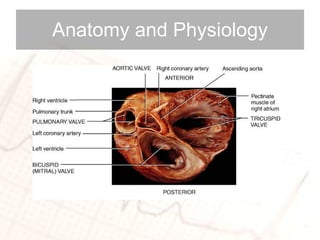
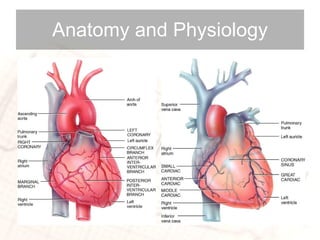
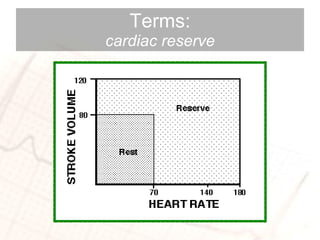
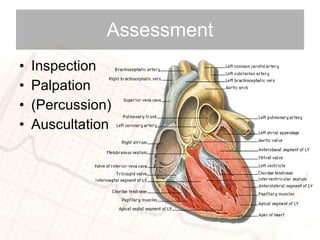
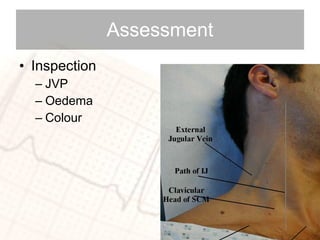
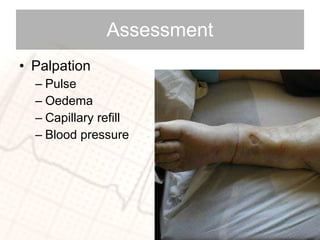
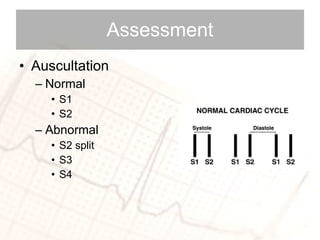
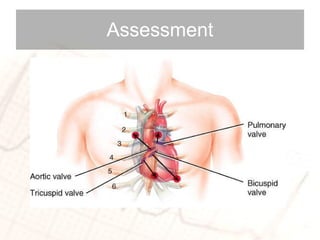
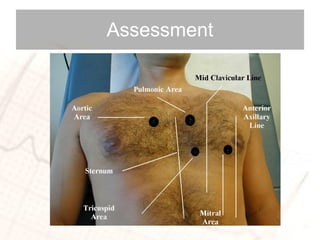
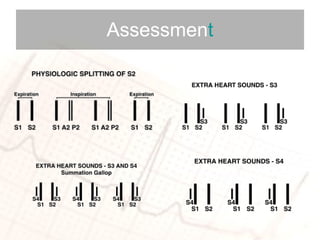
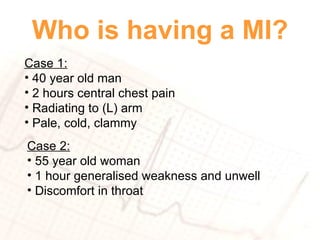
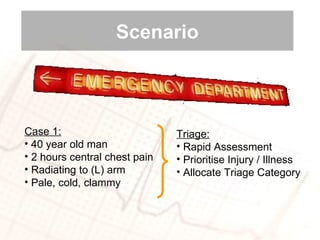
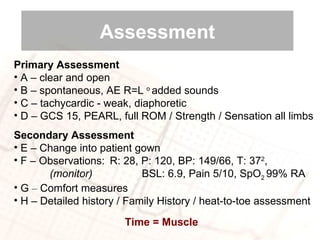
The document discusses cardiac anatomy and physiology. It describes the heart's location in the chest, its layers including the pericardium, myocardium and endocardium. It lists the four heart valves that control blood flow and terms related to heart function such as stroke volume and cardiac output. Assessment techniques for the heart like inspection, palpation and auscultation are also mentioned along with common causes of chest pain and risk factors for heart disease.


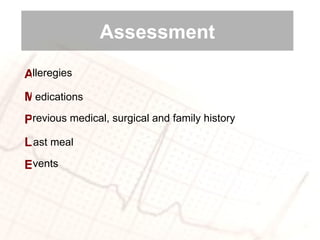
![osition: Where is the Pain? P Q R S T A A A uality: What does the pain feel like? [sharp, dull, burning] adiation: Does the pain move anywhere? everity: Rate the pain on a scale between 0 and 10 iming: When did the pain start? Is it continuous? lleviating factors: What makes it better? ggravating factors: What makes it worse? ssociated symptoms: e.g., nausea / pins and needles Assessment](https://image.slidesharecdn.com/cardiacap-100608185330-phpapp01/85/Cardiac-Anatomy-and-Physiology-38-320.jpg)