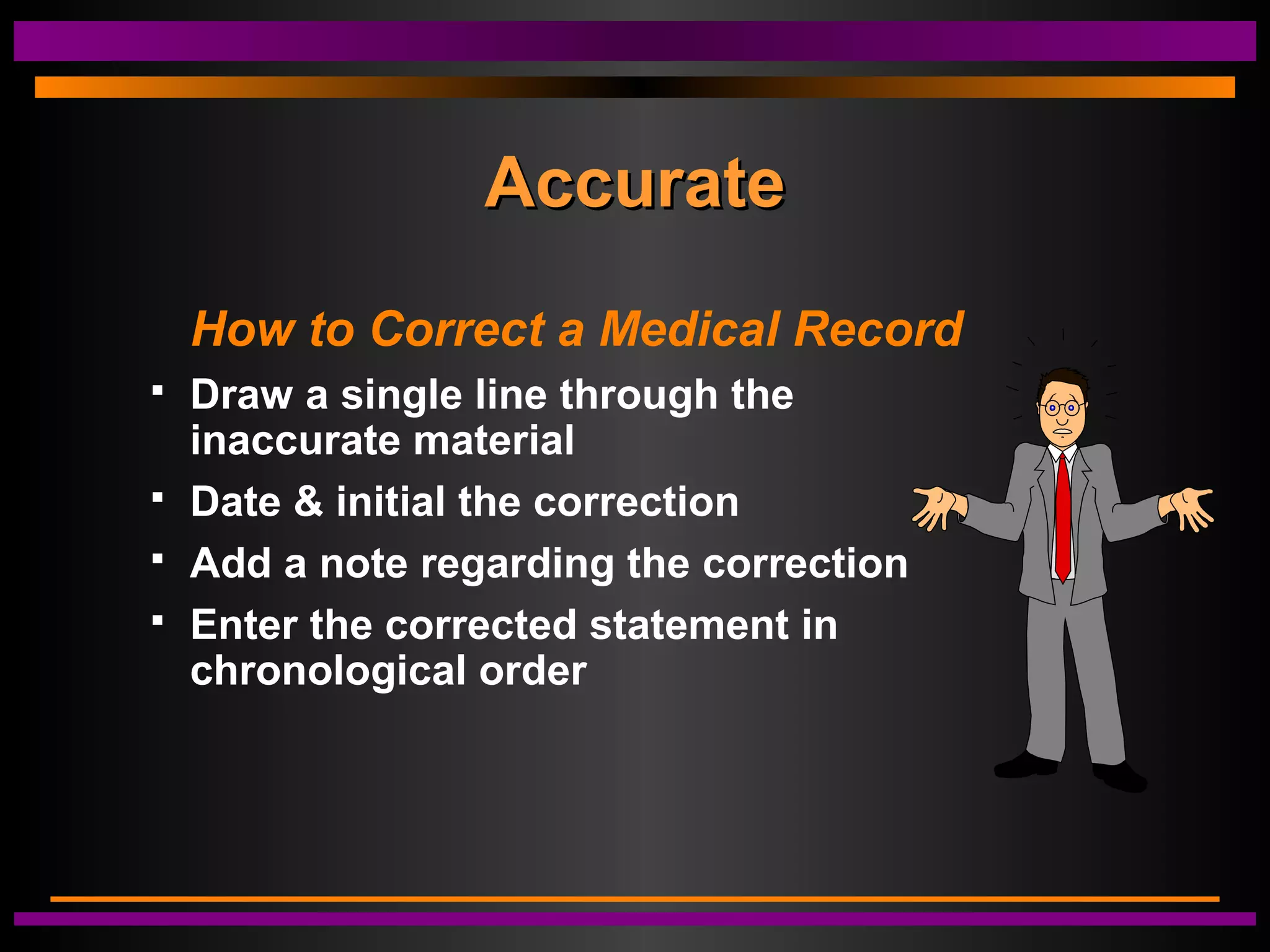
This document discusses the importance of proper medical documentation. It begins by defining medical documentation and outlining its key purposes, which include preserving patient information, justifying treatment, allowing for continuity of care, and satisfying regulatory requirements. The document emphasizes that documentation must be accurate, complete, legible, objective, and free of extraneous information. It differentiates between objective clinical findings and subjective patient-reported information. Proper documentation is presented as important for patient care, risk management, and legal protection for medical professionals.