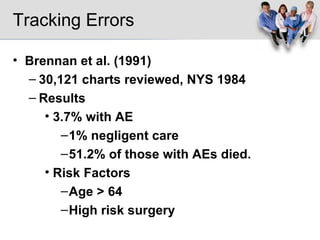
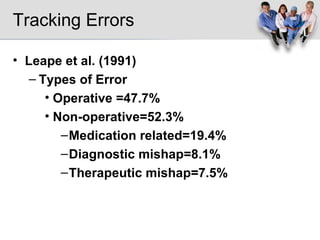
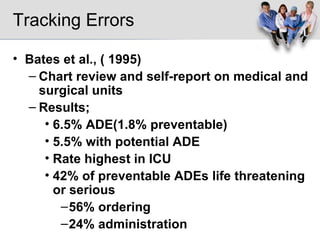
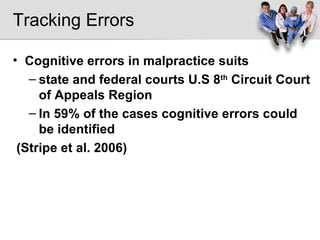
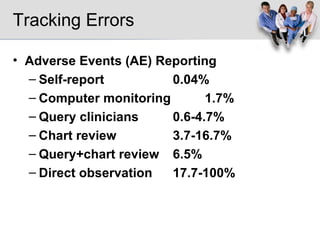
1. The document discusses various methods that have been used to track and reduce medical errors, including chart reviews, self-reporting, and direct observation. Errors are often caused by systemic issues rather than individual mistakes.
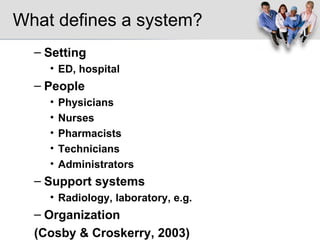
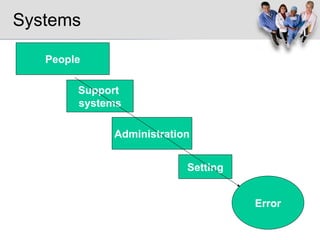
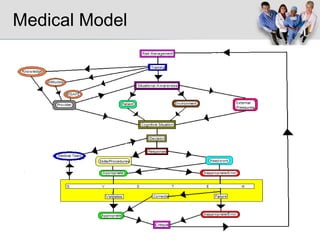
2. A systems approach aims to identify error sources within healthcare systems and implement solutions like checklists, improved teamwork, and computerized physician order entry.
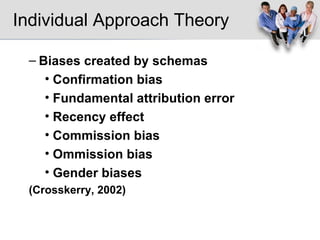
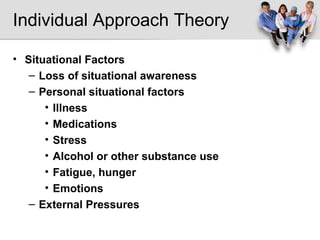
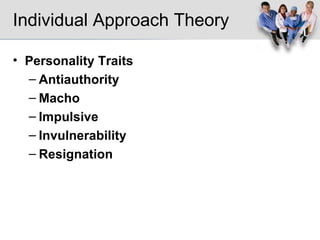
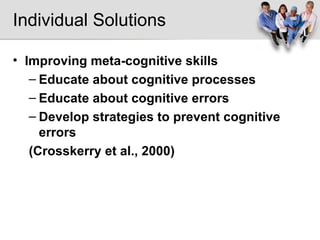
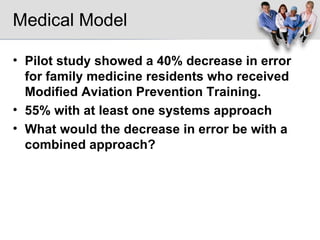
3. An individual approach provides education to improve cognitive skills and decision-making and reduce biases. Integrating systems solutions and cognitive training shows promise but requires more research.