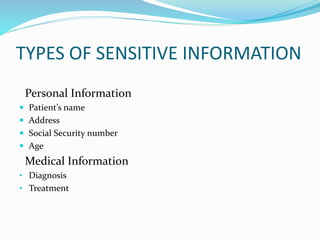
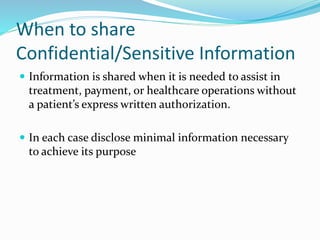
Confidentiality refers to sensitive information that is given privately and not intended to be shared. This document outlines what types of information are considered sensitive, such as names, medical diagnoses, and treatment details. It discusses when limited sharing is allowed, such as for treatment purposes, and emphasizes disclosing only necessary minimal information. Guidelines are provided for handling media inquiries, anonymizing data where possible, and obtaining consent before disclosure. Laws like HIPAA create barriers to restrict unauthorized access to protected health information. Accountability and penalties are important to maintain patient trust. Software and policies aim to safeguard information access and detect misuse.