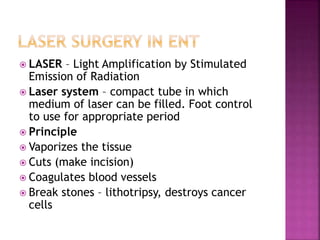
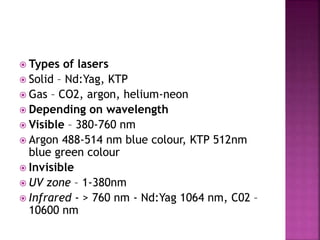
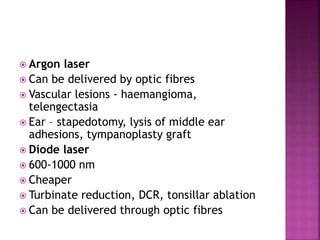
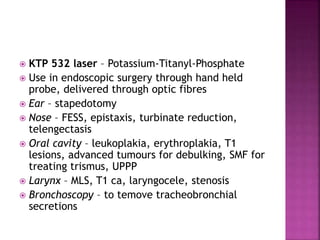
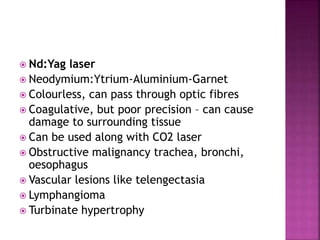
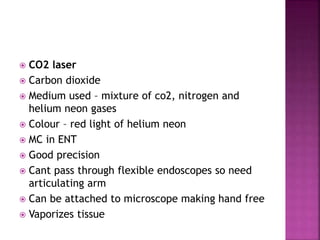
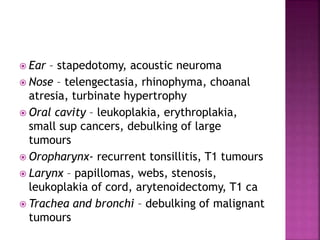
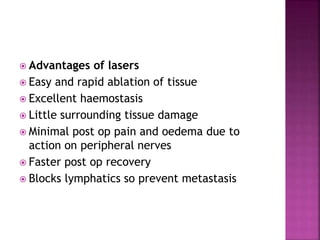
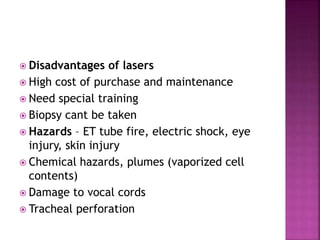
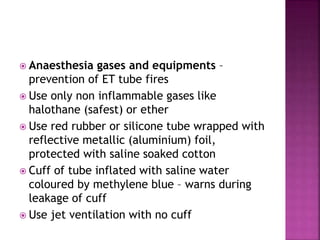
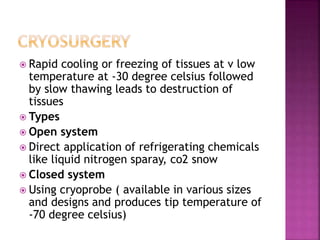
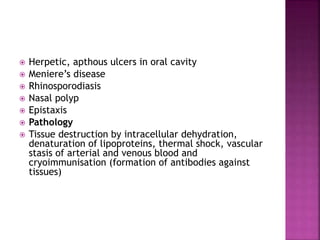
The document discusses various laser and cryosurgery techniques used in ENT. It describes how lasers like CO2, KTP, and Nd:YAG use light amplification to cut, coagulate, and ablate tissue. Cryosurgery uses rapid freezing to below -30°C followed by slow thawing to destroy tissues. Both techniques are used to treat lesions, tumors, and other ENT conditions. Safety precautions are important as these techniques can damage surrounding normal tissues if not properly administered.