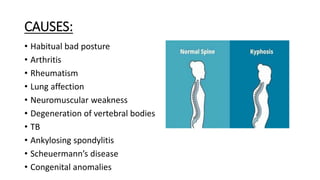
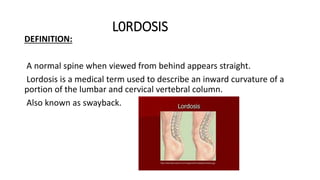
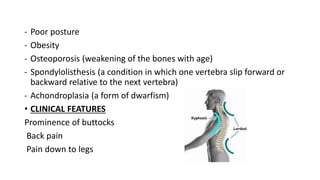
The document discusses kyphosis, a spinal disorder characterized by an excessive outward curve of the spine, and lordosis, an inward curvature of the lumbar and cervical regions. It details the types, causes, symptoms, and treatment options for both conditions, emphasizing the importance of physical therapy, ergonomic adjustments, and in some cases, bracing or surgery. Kyphosis commonly arises from postural issues or age-related factors, while lordosis may result from obesity, congenital issues, or trauma.