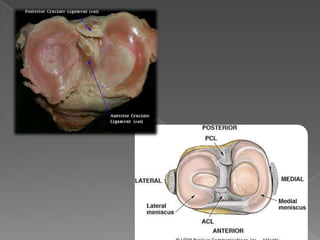
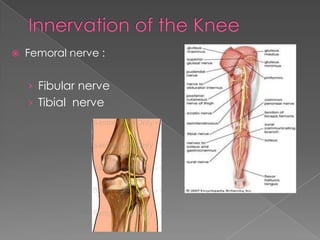
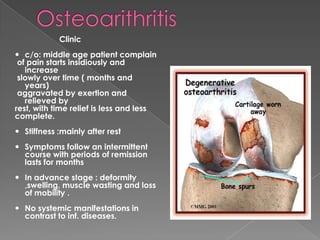
The knee joint is the largest and most complicated joint in the body. It consists of three joints within a single synovial cavity: the medial and lateral condylar joints between the femur and tibia, and the patellofemoral joint between the patella and femur. The knee joint is supported by ligaments such as the ACL and PCL, as well as menisci. Osteoarthritis is a common condition affecting the knee joint, characterized by the progressive destruction of articular cartilage and new bone growth, leading to pain and stiffness. It results from an imbalance between mechanical stress on the cartilage and its ability to withstand that stress.