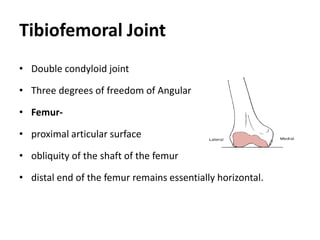
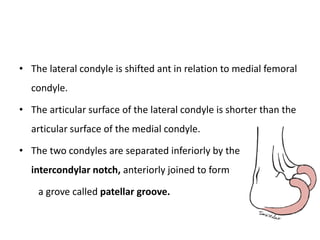
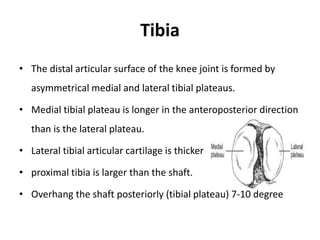
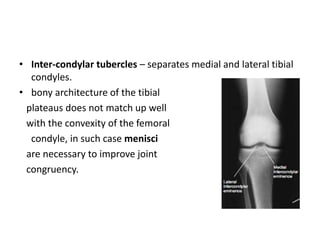
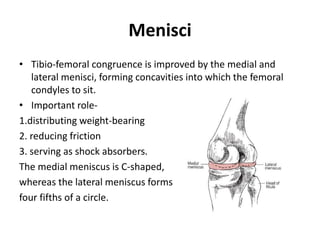
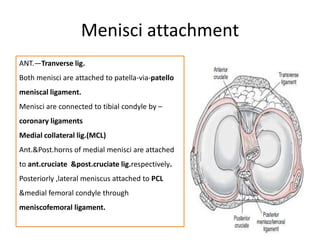
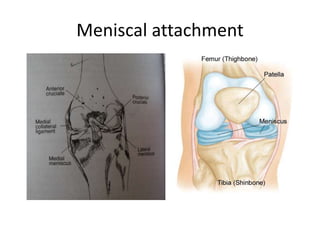
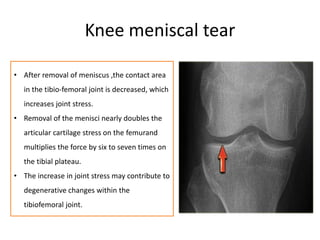
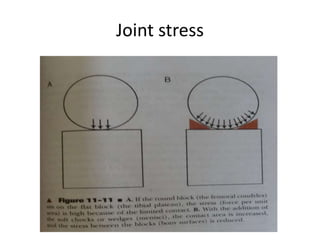
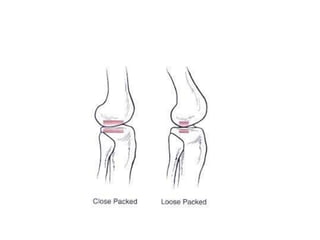
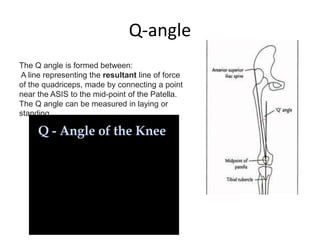
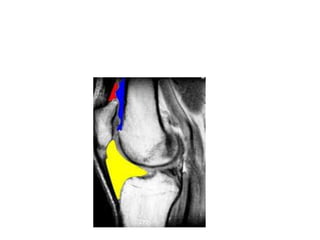
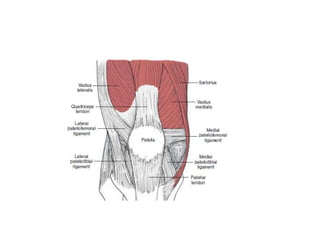
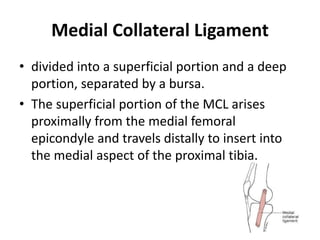
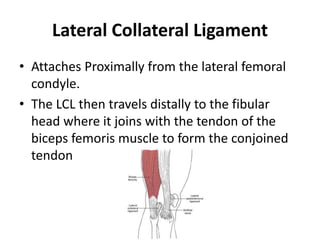
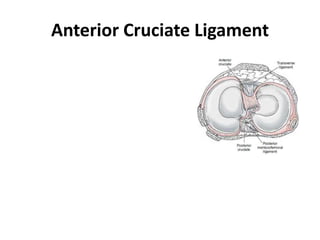
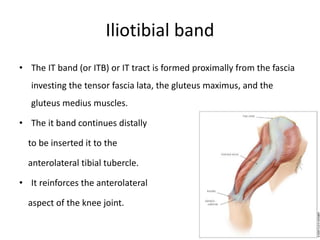
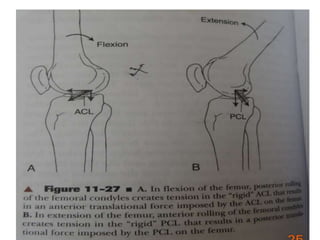
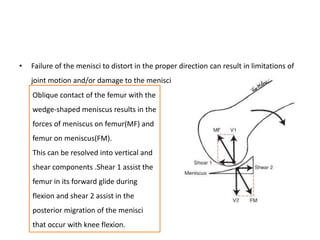
The knee joint is composed of two articulations, the tibiofemoral joint and patellofemoral joint. The tibiofemoral joint allows 3 degrees of freedom of motion and contains the femoral condyles which articulate with the menisci and tibial plateaus. The menisci improve joint congruence and distribute weight forces. Ligaments such as the ACL, PCL, MCL and LCL provide stability to the joint. The patellofemoral joint contains the patella which articulates with the femur and is stabilized by surrounding structures like the quadriceps tendon.