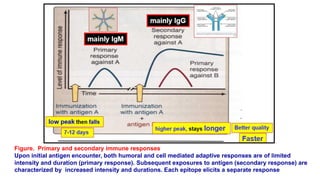
The immune system protects the body from pathogens through innate and adaptive immunity. Innate immunity provides immediate protection through physical barriers, inflammation, and phagocytosis. Adaptive immunity has antigen-specific responses and immunological memory. It involves B cells producing antibodies and T cells that mediate cellular immunity. Hypersensitivities occur when the immune system overreacts to antigens, potentially causing tissue damage.