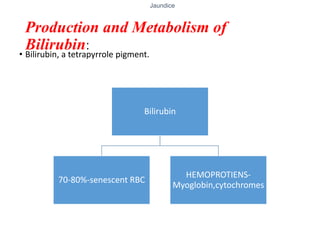
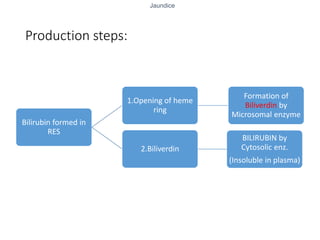
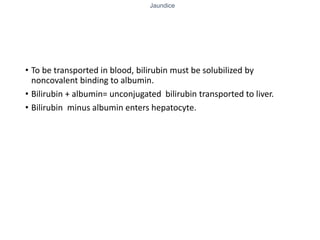
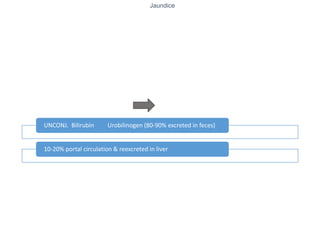
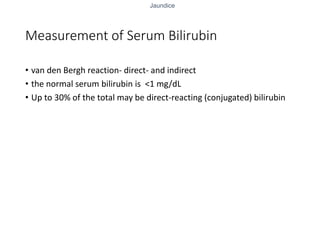
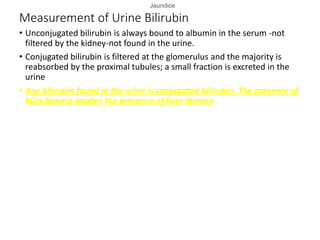
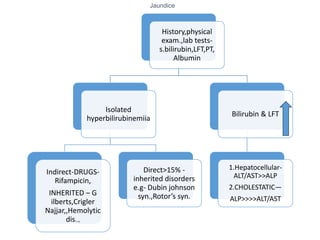
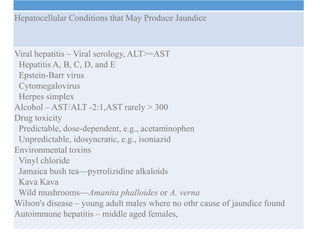
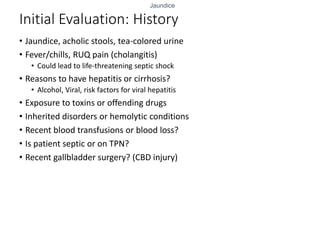
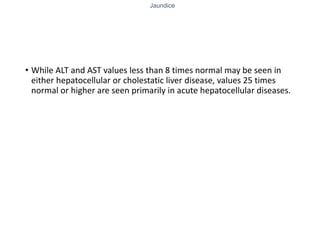
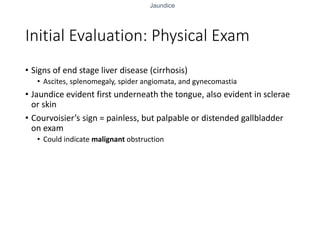
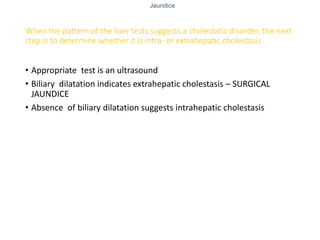
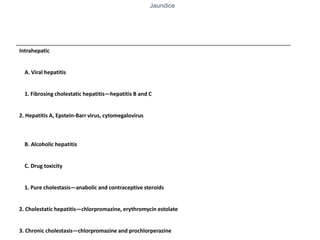
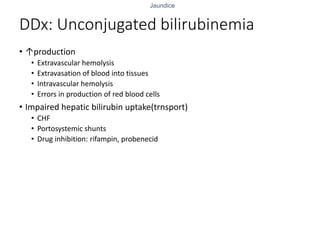
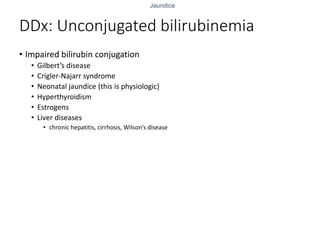
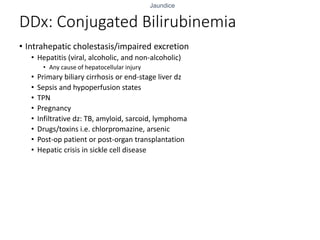
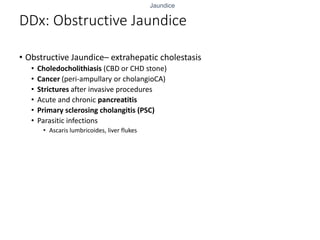
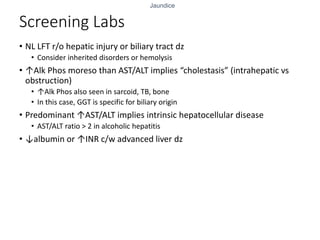
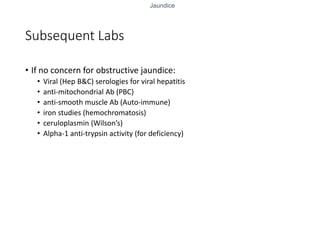
Jaundice is caused by increased levels of bilirubin in the blood which deposits in tissues, causing a yellowish discoloration. It is detected by examining the sclerae. Jaundice can be unconjugated resulting from increased bilirubin production or impaired liver function, or conjugated due to obstruction of the bile ducts. Evaluation of a patient with jaundice includes history, physical exam, liver function tests, and imaging to determine if the cause is hepatocellular injury or obstruction. Treatment depends on identifying and addressing the underlying etiology such as viral hepatitis, gallstones, or cancer.