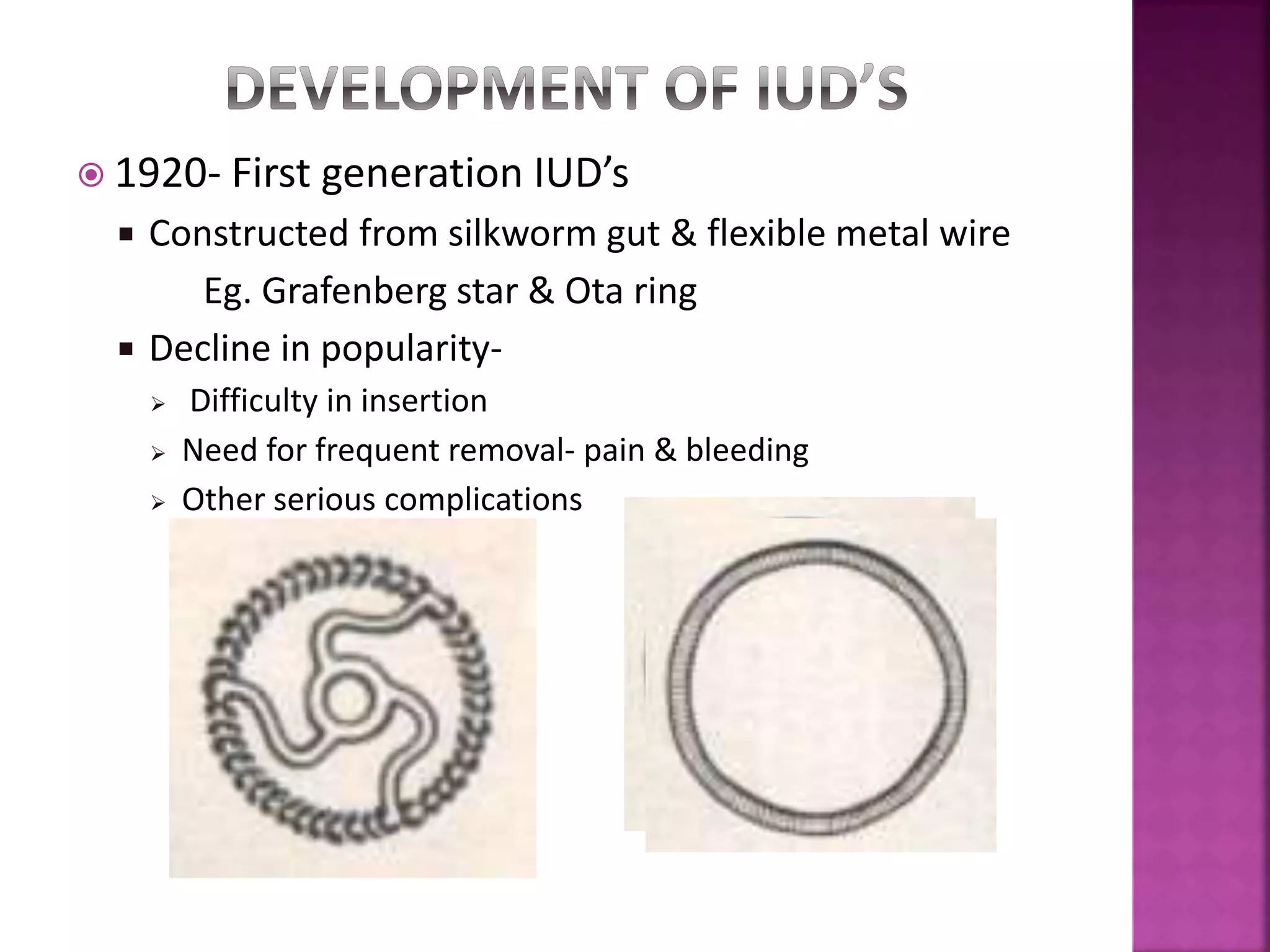
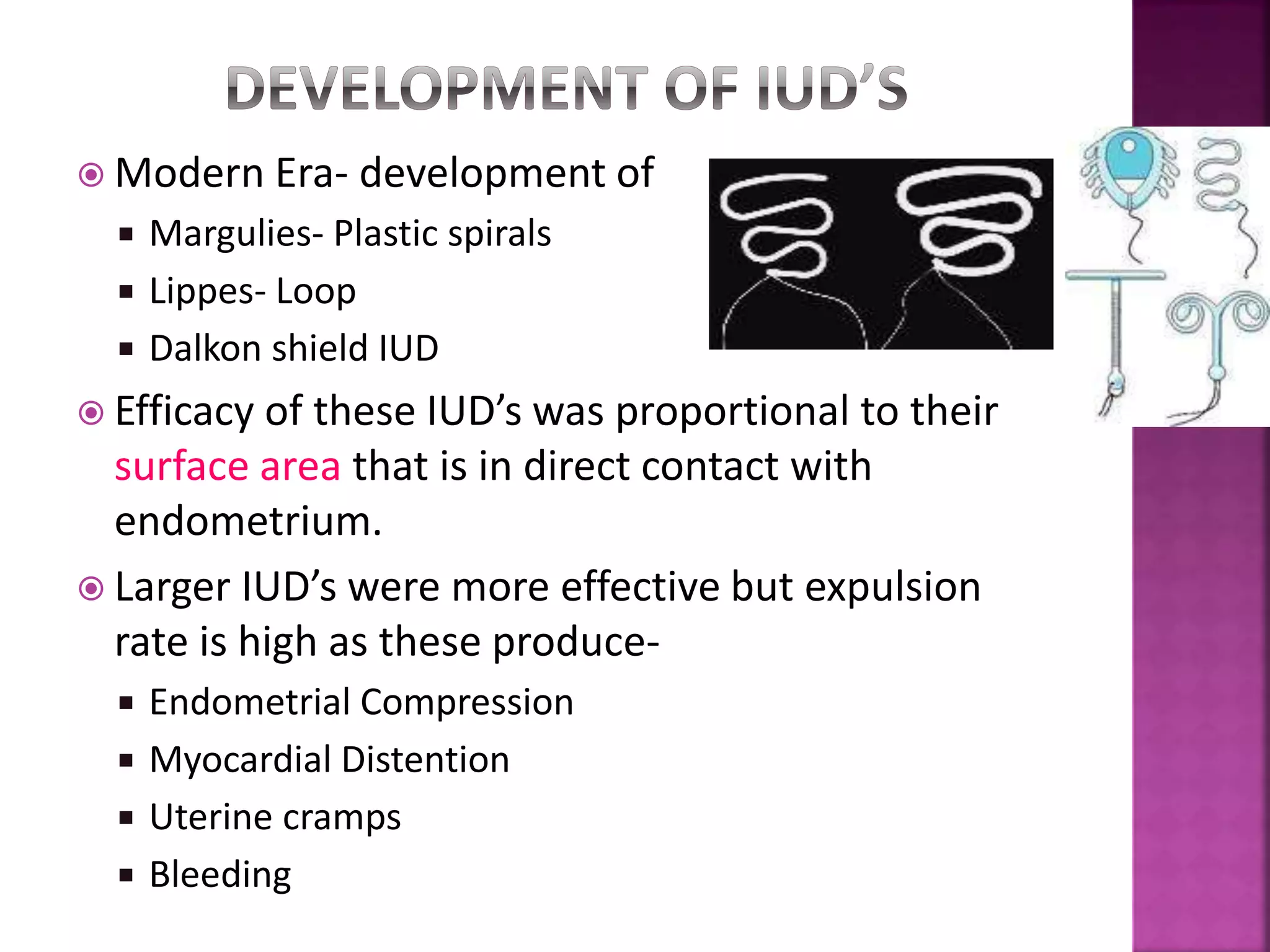
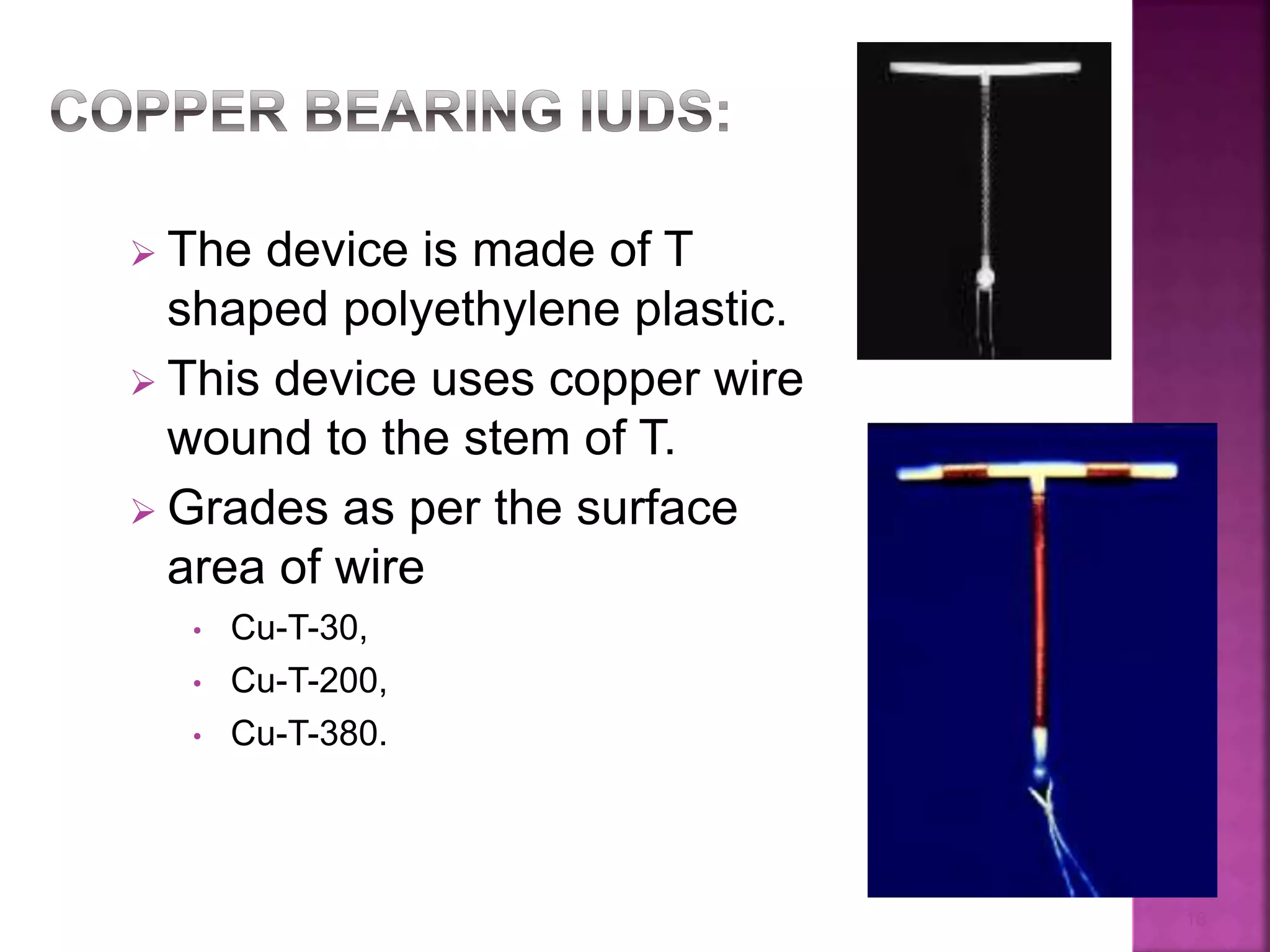
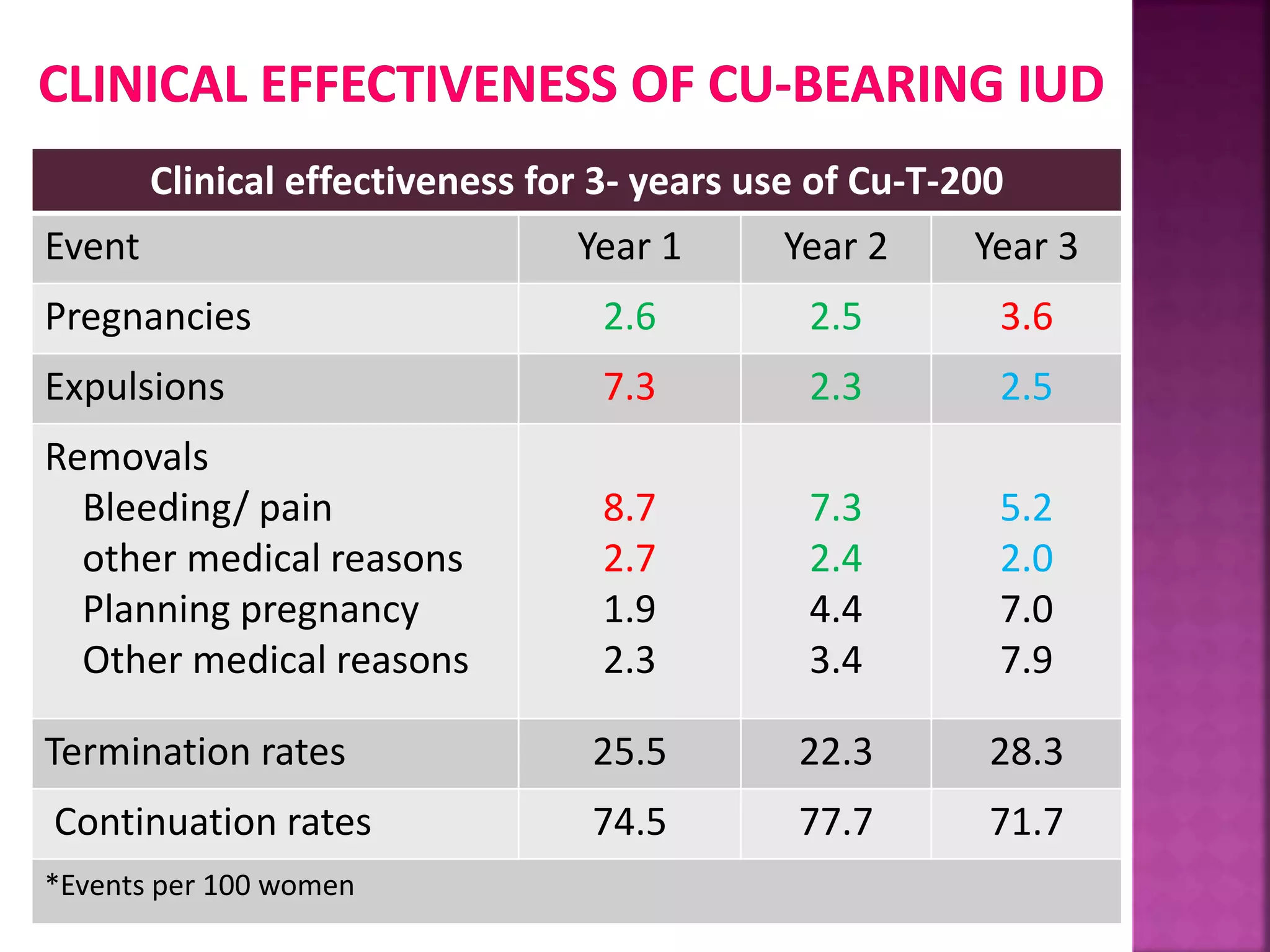
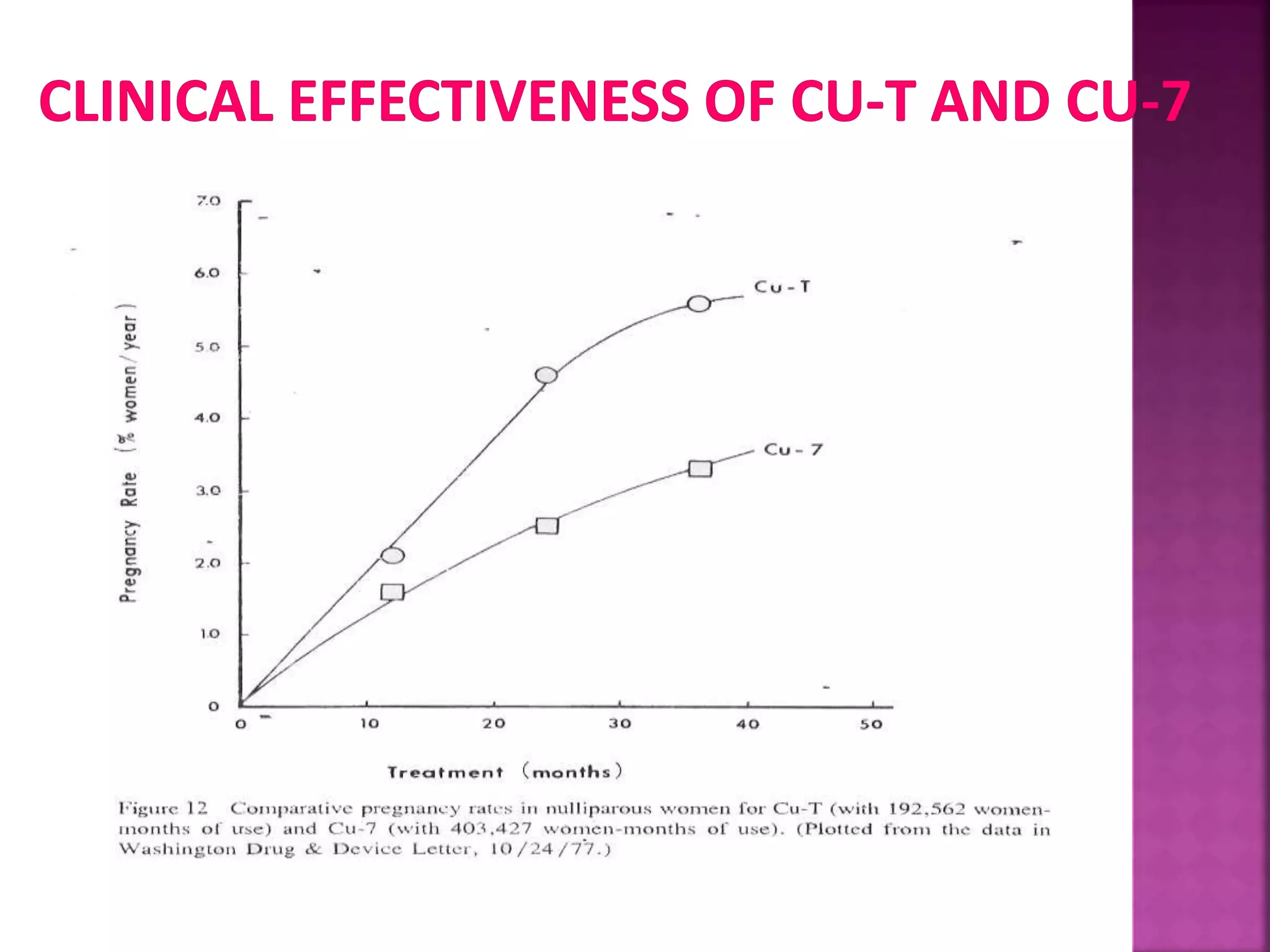
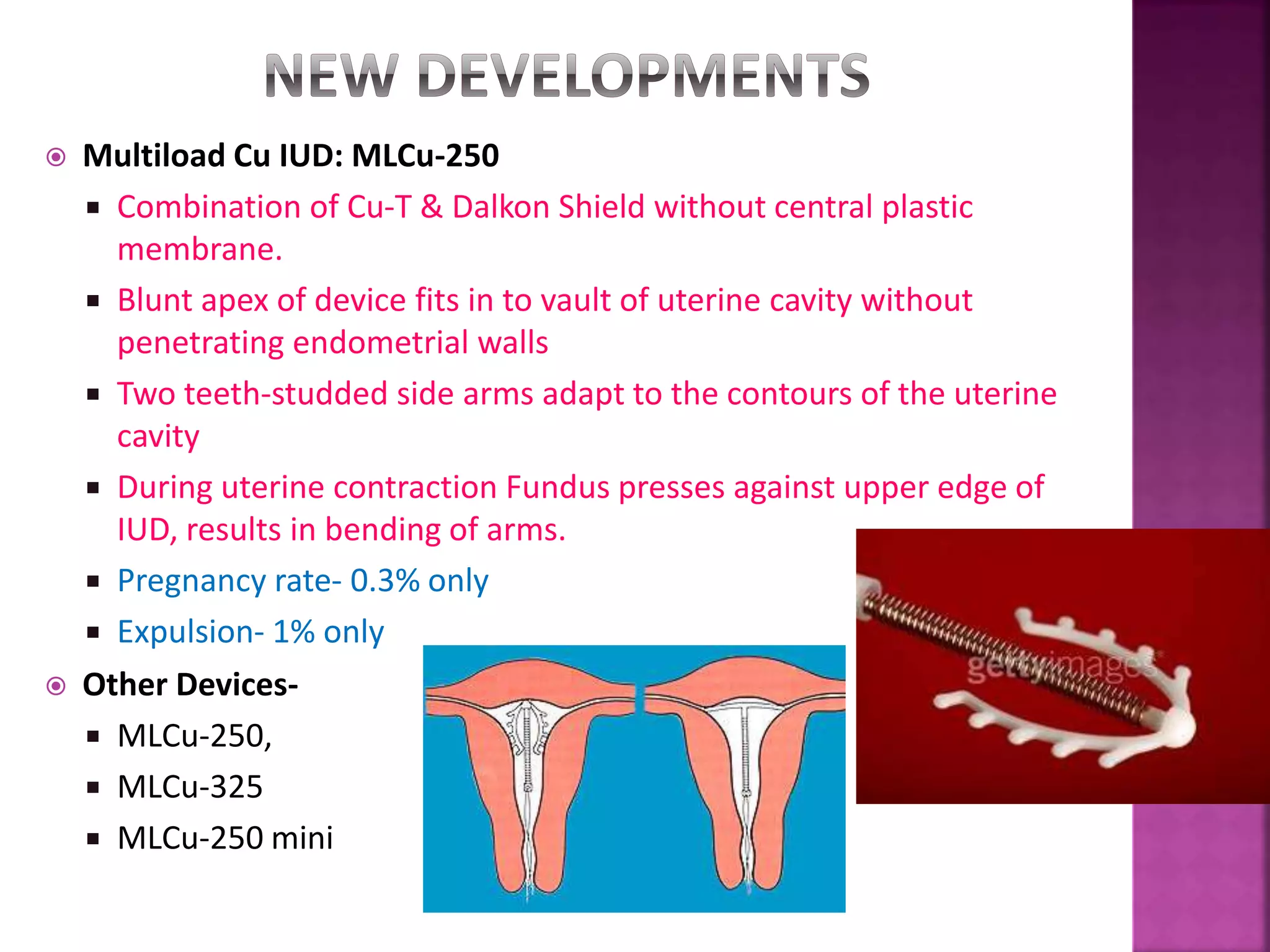
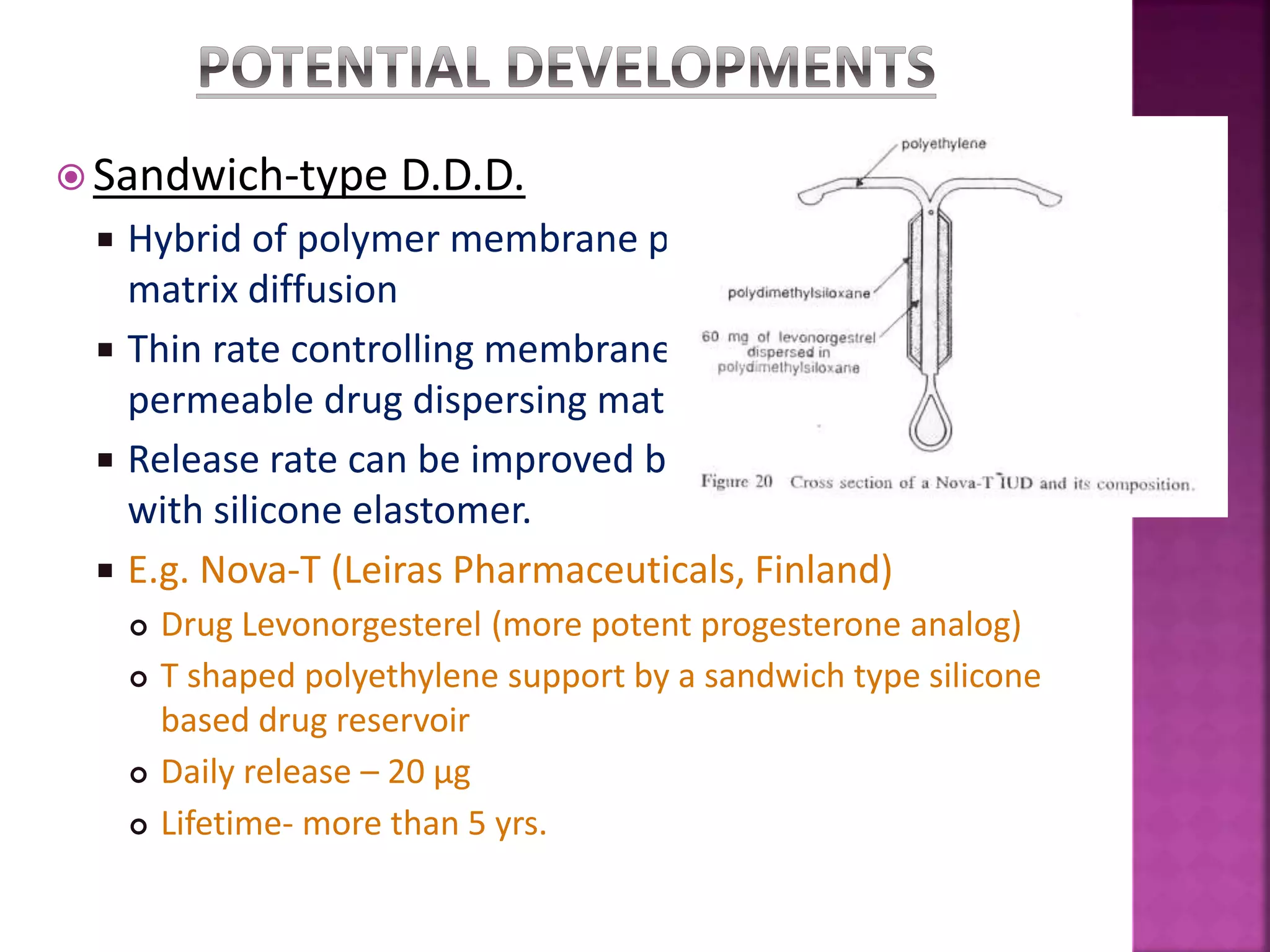
This document discusses intrauterine devices (IUDs) as a form of contraception. It begins with an introduction to contraception and the anatomy of the uterus. It then discusses the history and development of IUDs, including early non-medicated IUDs made of materials like plastic and copper-bearing IUDs that enhance effectiveness. The document outlines the types of modern IUDs, including copper IUDs and hormone-releasing IUDs. It compares the efficacy of medicated versus non-medicated IUDs and discusses new developments in long-acting IUD designs.