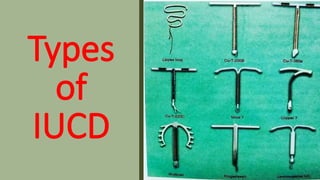
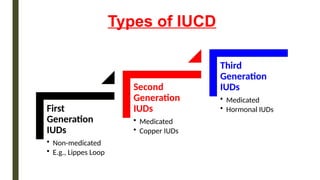
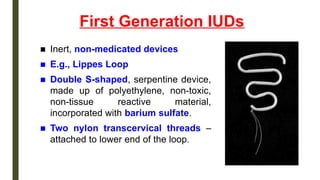
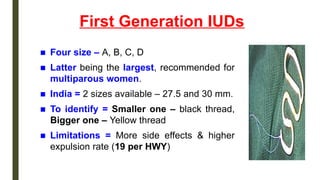
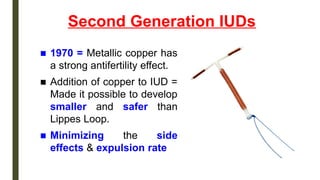
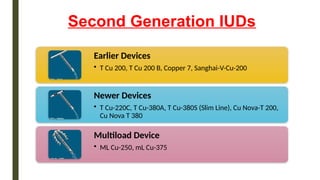
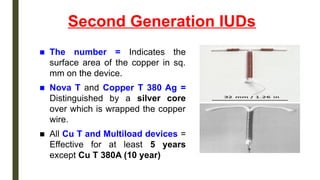
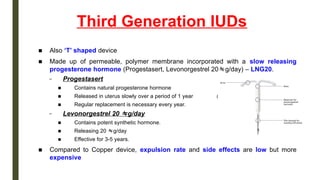
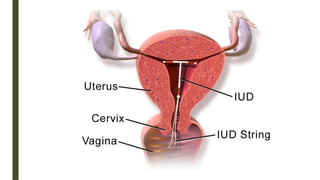
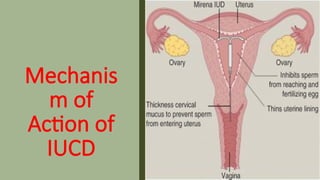
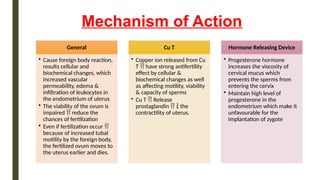
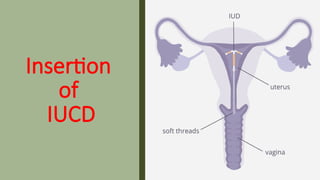
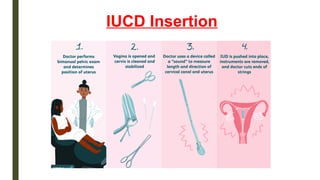
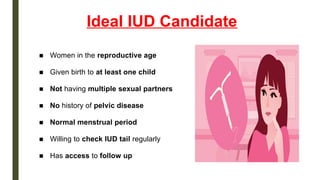
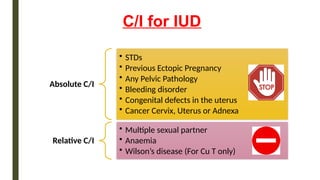
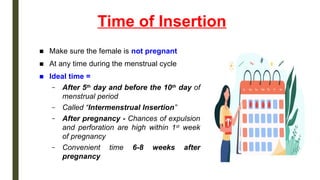
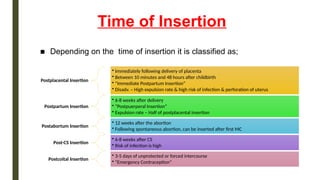
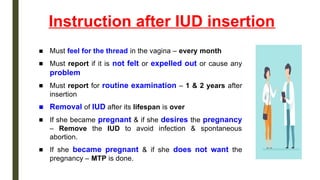
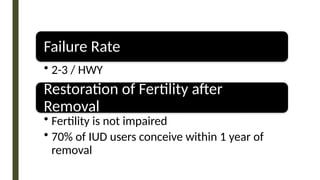
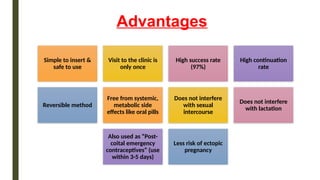
The document provides an overview of intrauterine contraceptive devices (IUDs), detailing their history, types (first, second, and third generation), mechanisms of action, ideal candidates, insertion timings, and post-insertion advice. It highlights the advantages such as high success rates and reversibility, as well as disadvantages including potential menstrual changes and risk of pelvic infection. Overall, it serves as a comprehensive guide on the use, effectiveness, and considerations regarding IUDs in contraception.