This document discusses cerebral aneurysms and subarachnoid hemorrhage. It provides details on:
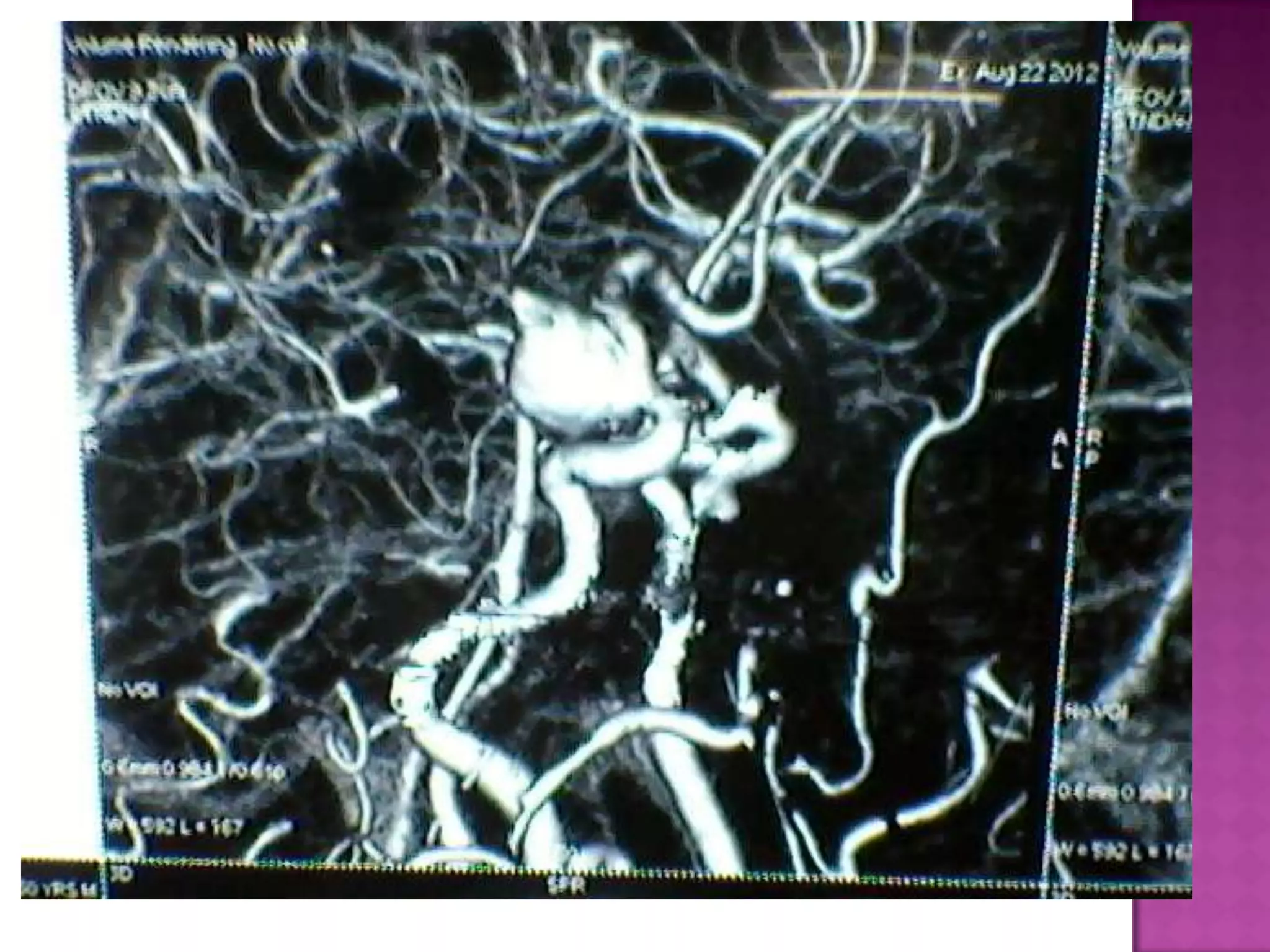
- The incidence, risk factors, locations, and causes of cerebral aneurysms
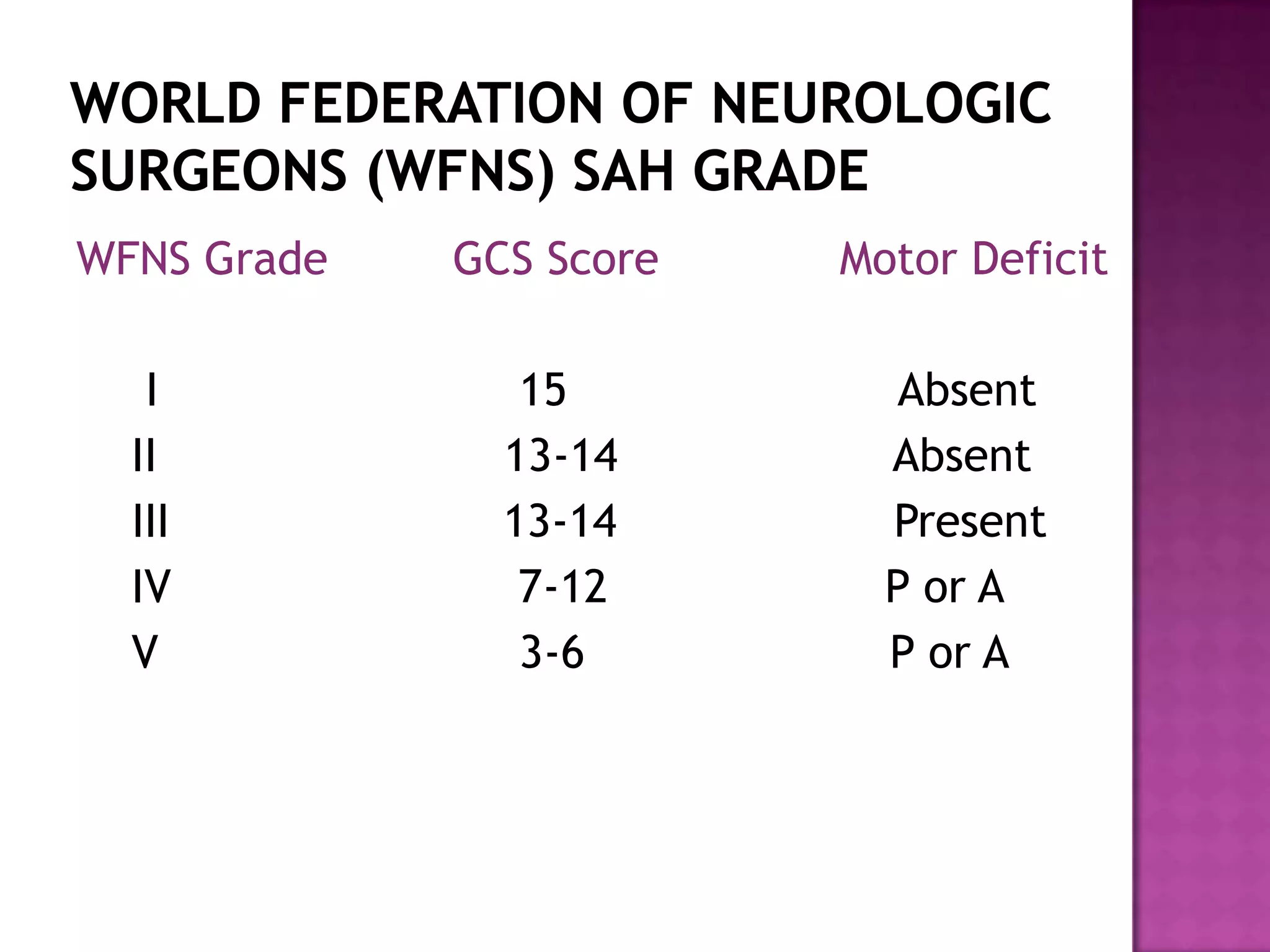
- Grading scales used to assess the severity of subarachnoid hemorrhage
- Complications associated with subarachnoid hemorrhage such as vasospasm, rebleeding, and elevated intracranial pressure
- Management strategies for unruptured and ruptured aneurysms including surgical clipping and endovascular coiling to prevent rebleeding