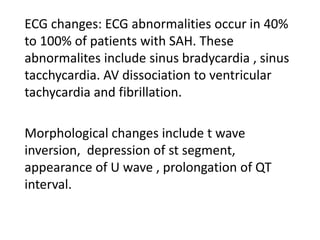
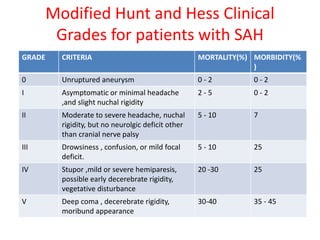
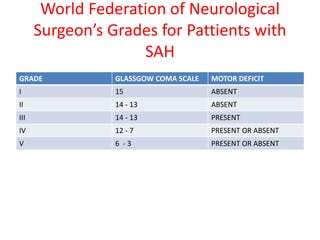
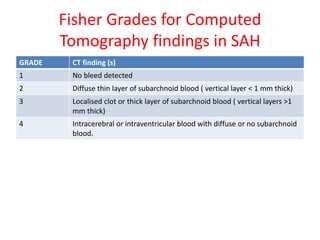
Subarachnoid hemorrhage is bleeding into the subarachnoid space surrounding the brain. It accounts for 5% of strokes but has high mortality and disability rates. The main causes are aneurysms (85%) and hypertension is a major risk factor. Patients present with sudden severe headache, vomiting, and possible loss of consciousness. Grading systems assess severity based on symptoms and imaging findings. Management involves stabilizing the patient, treating complications, and potentially clipping or coiling the aneurysm to prevent rebleeding. Anesthesia aims to control blood pressure rises during intubation and carefully monitor the patient.