The document summarizes the anatomy and physiology of the liver and biliary system. It describes:
1. The liver's dual secretory and excretory functions, and its location in the abdomen.
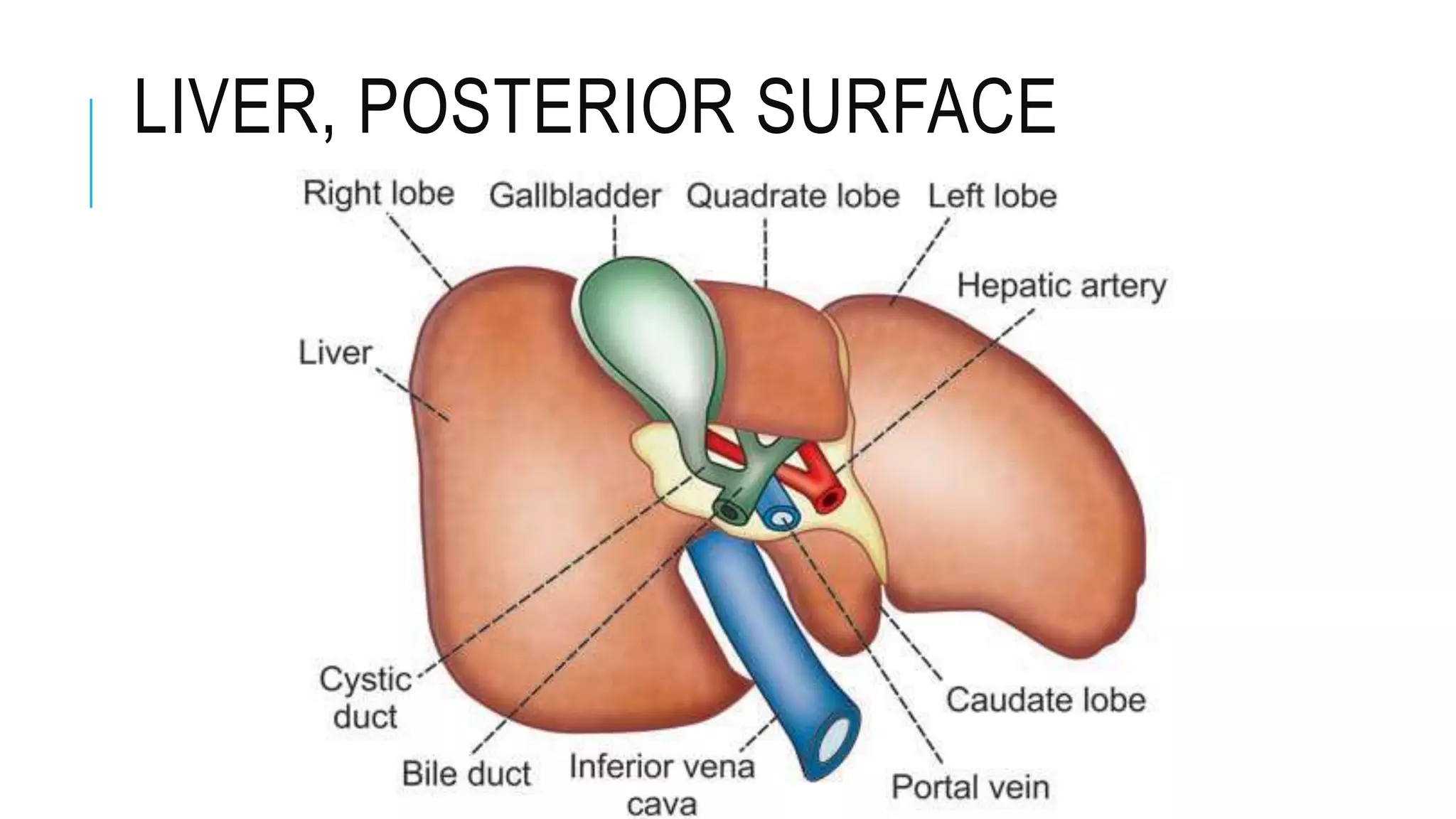
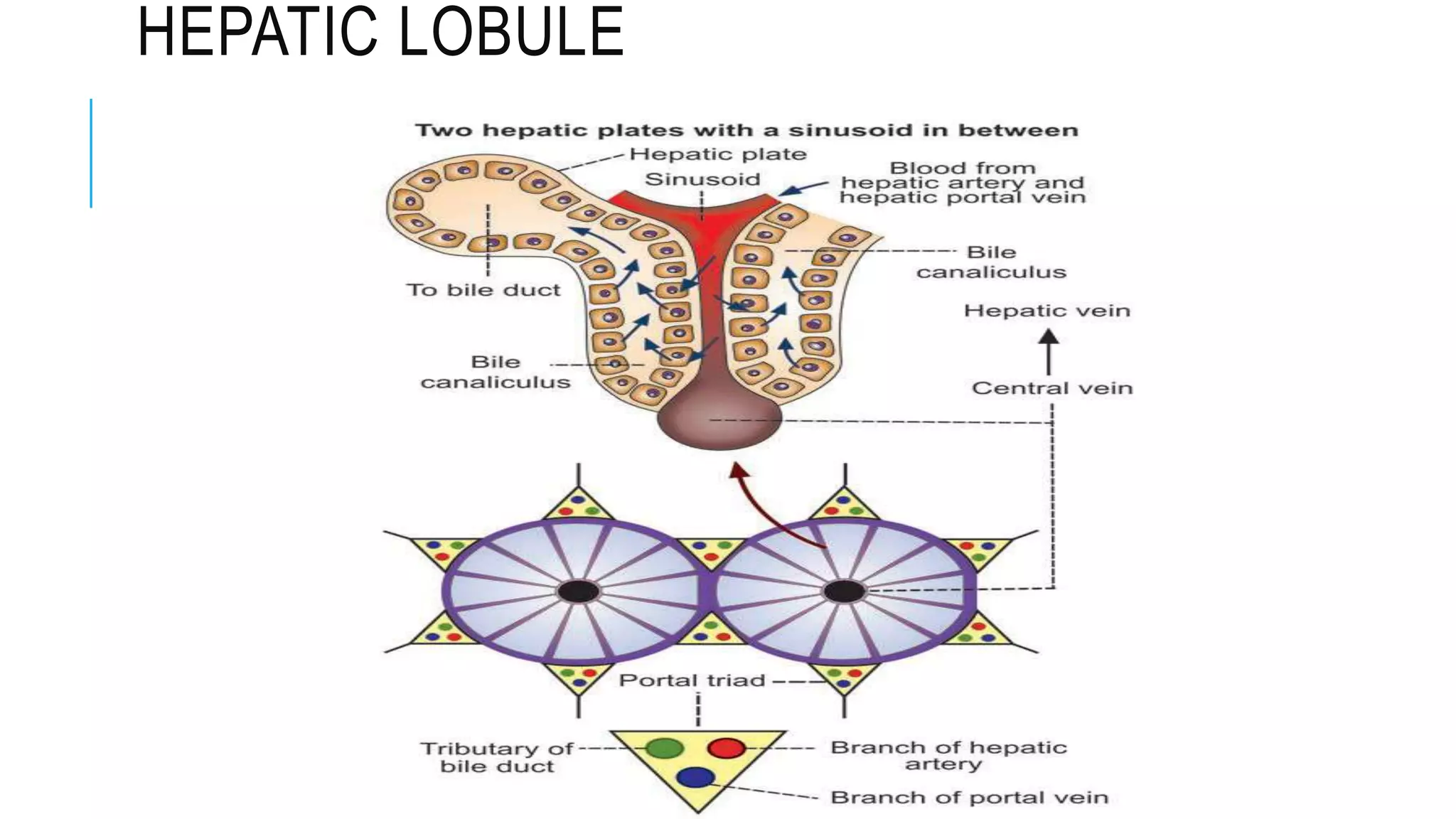
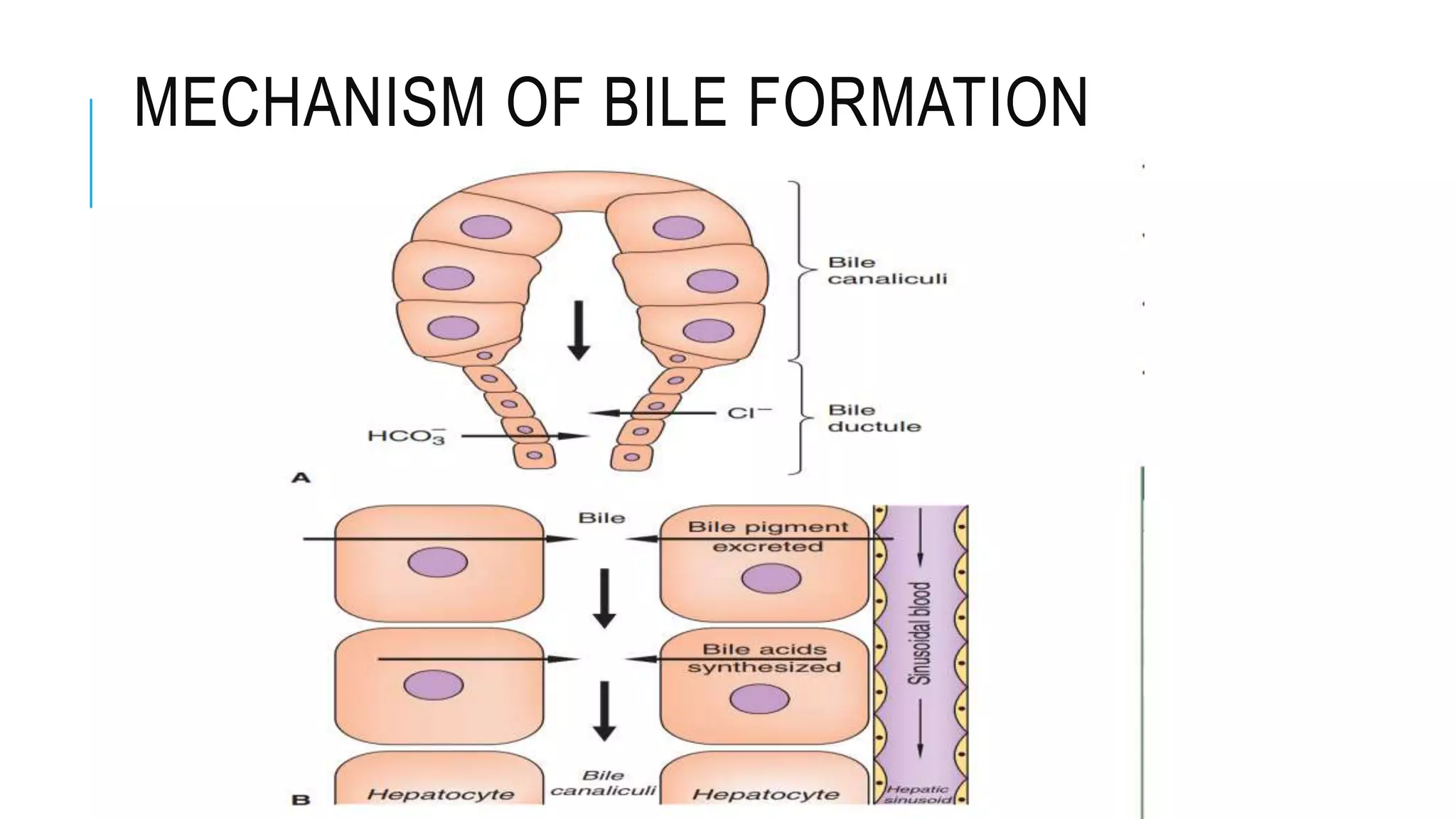
2. The hepatic lobes, lobules, hepatocytes, and bile canaliculi that make up the liver's structure.
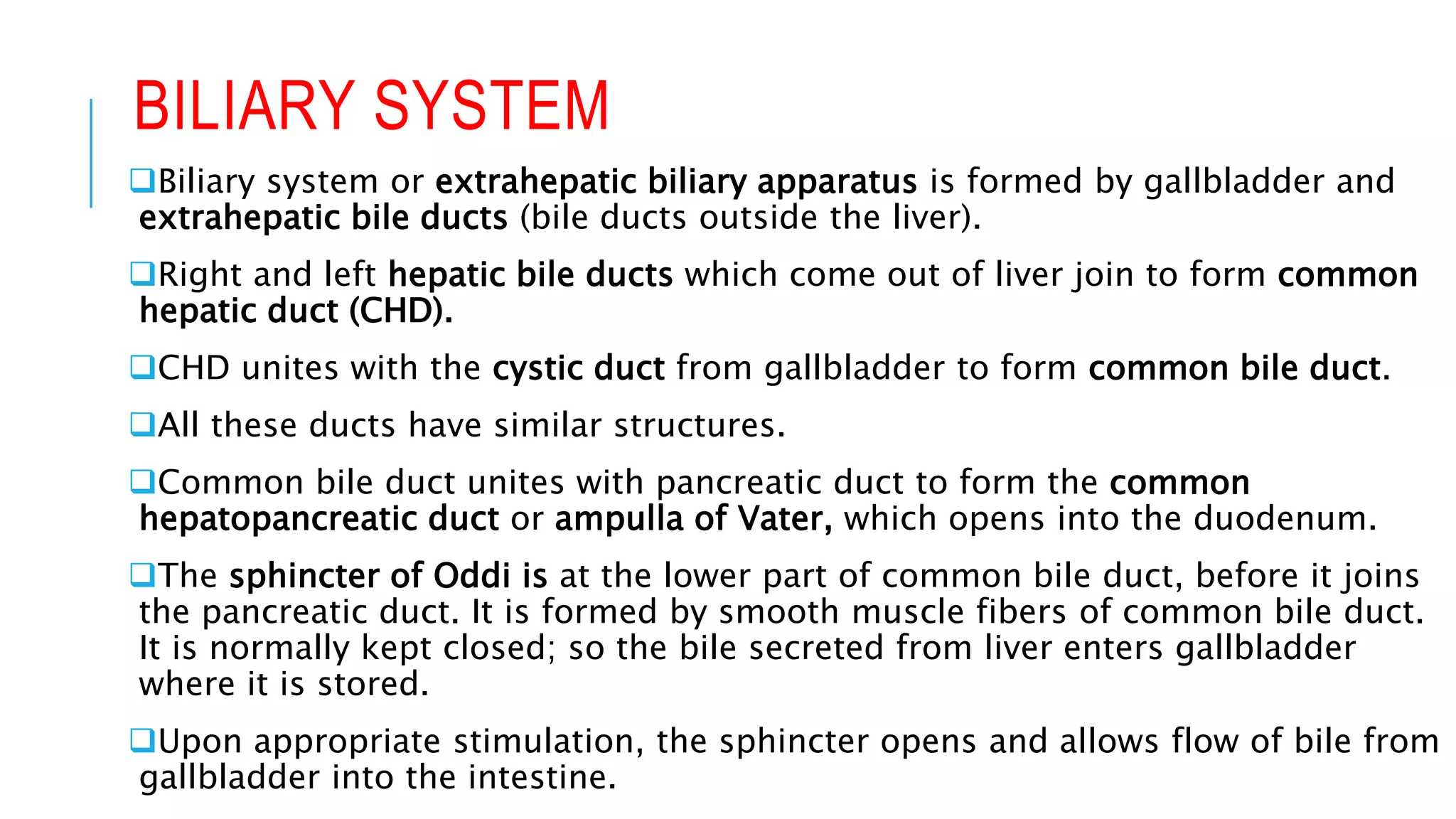
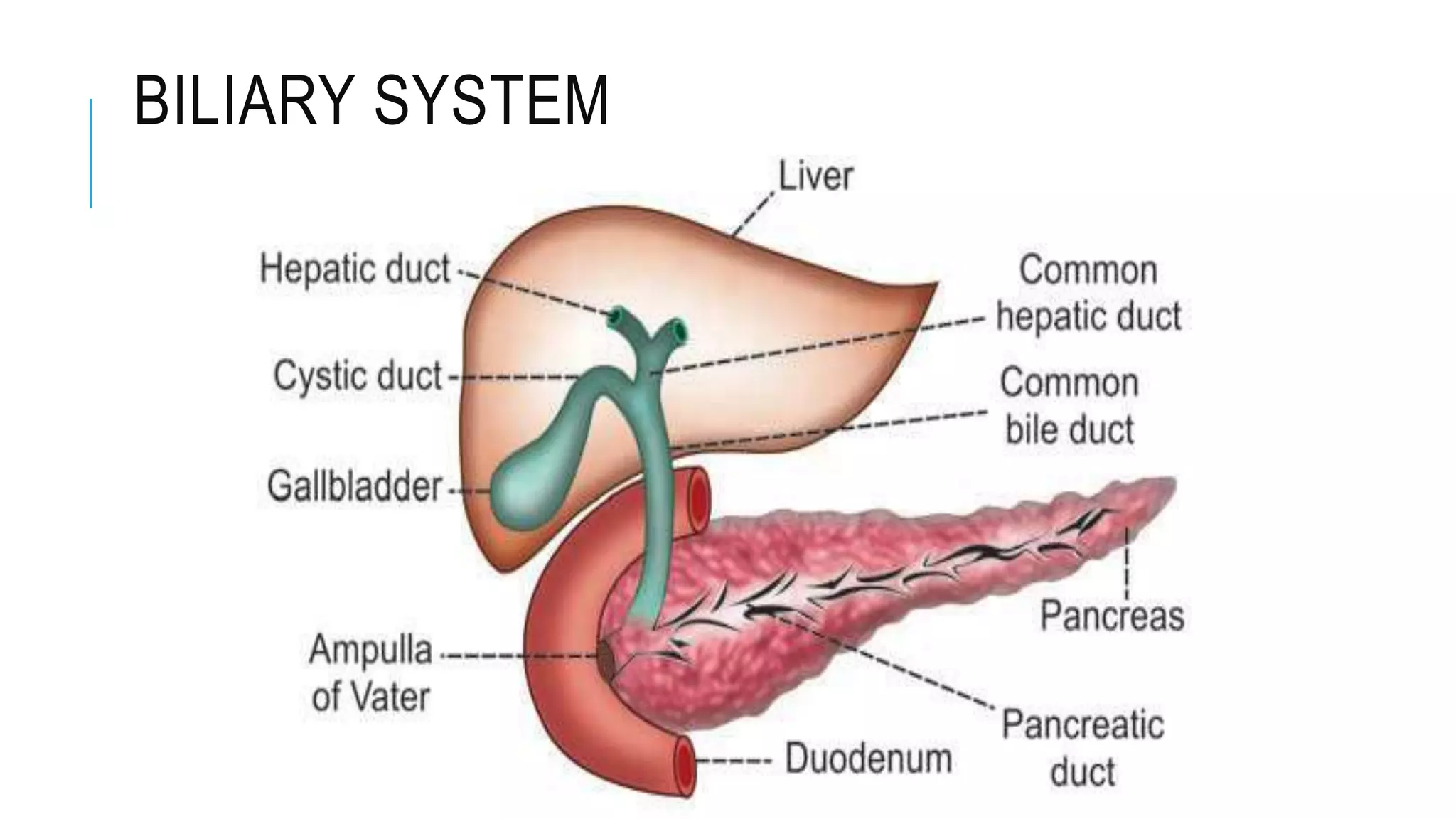
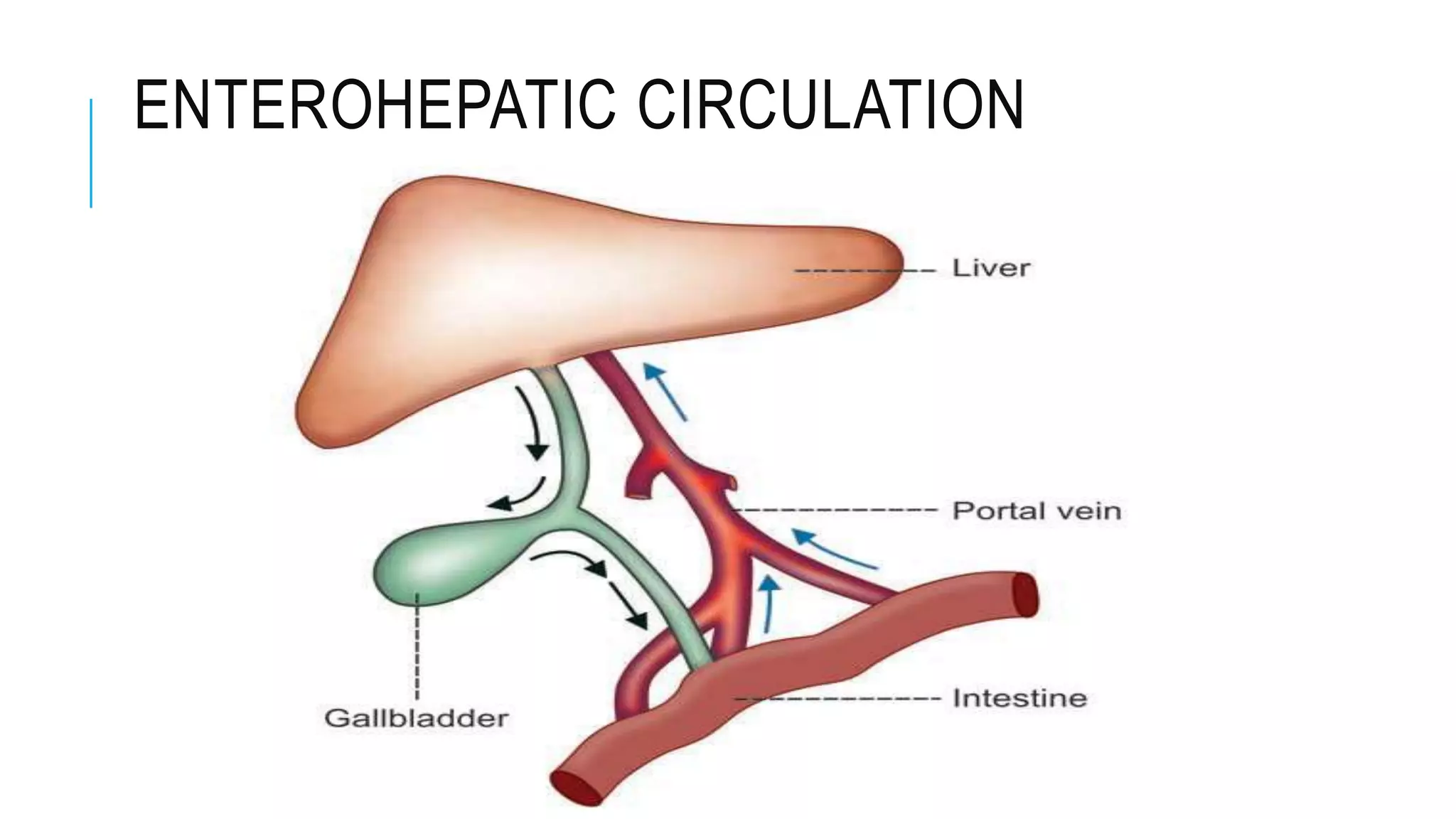
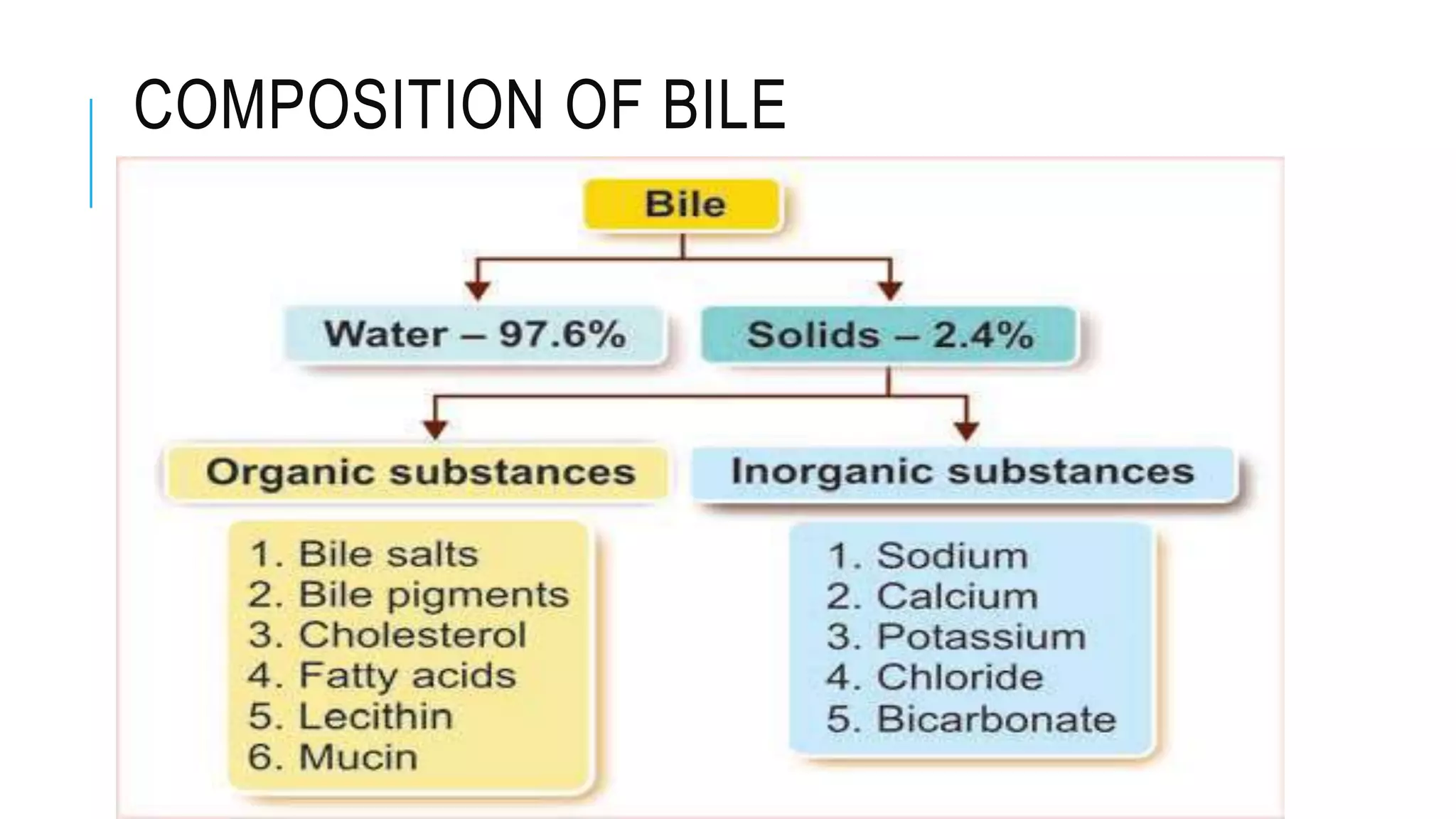
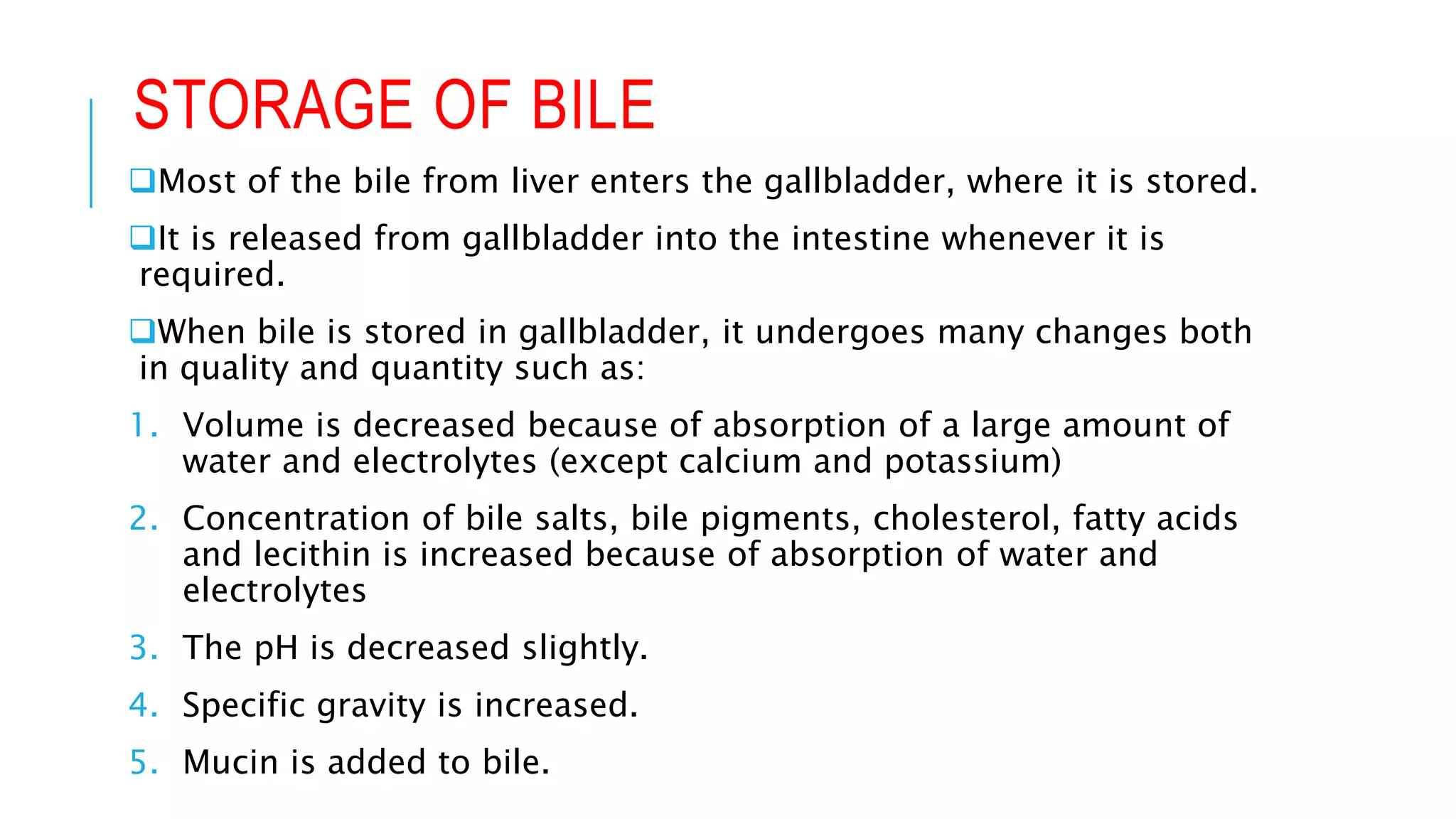
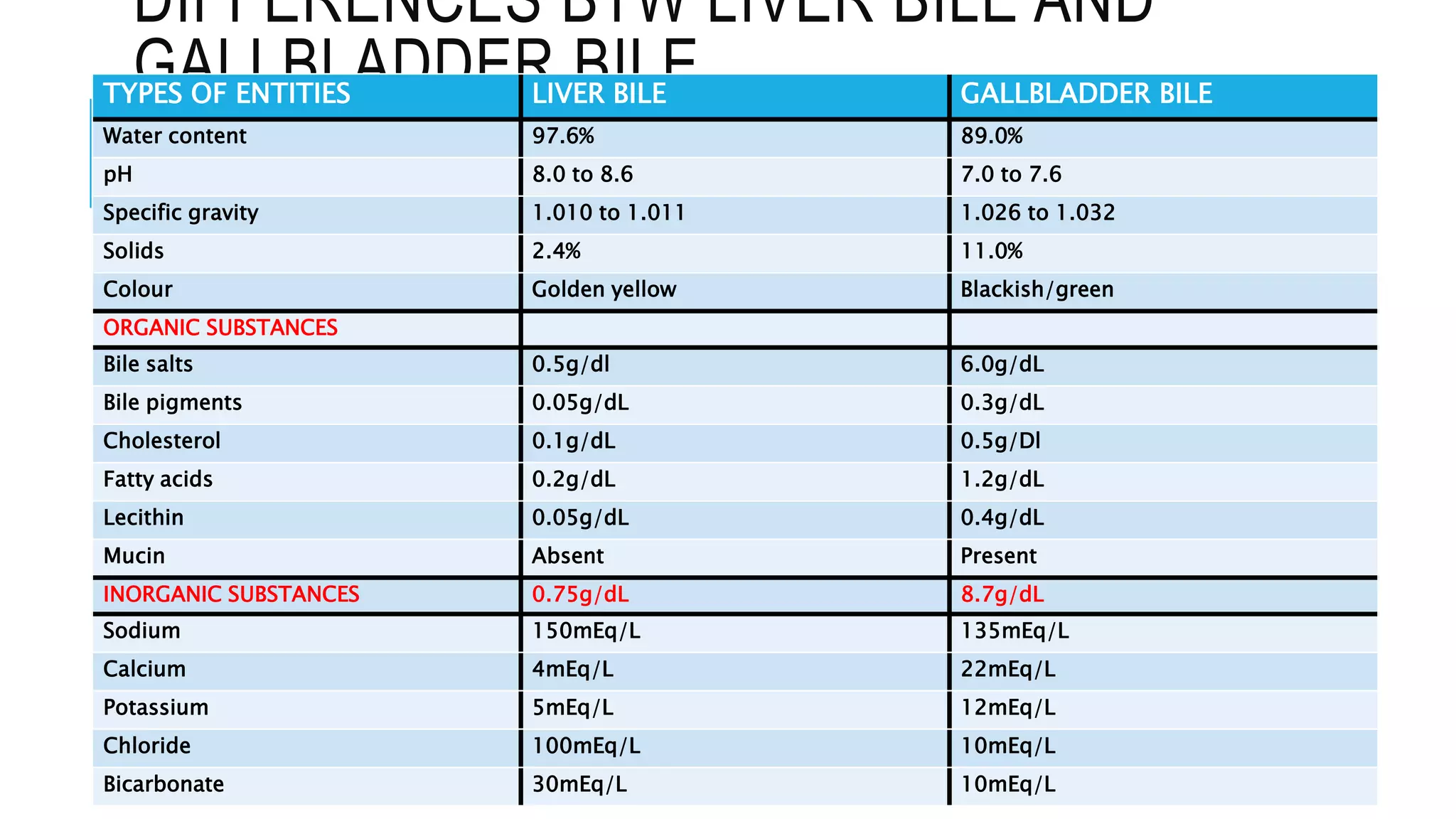
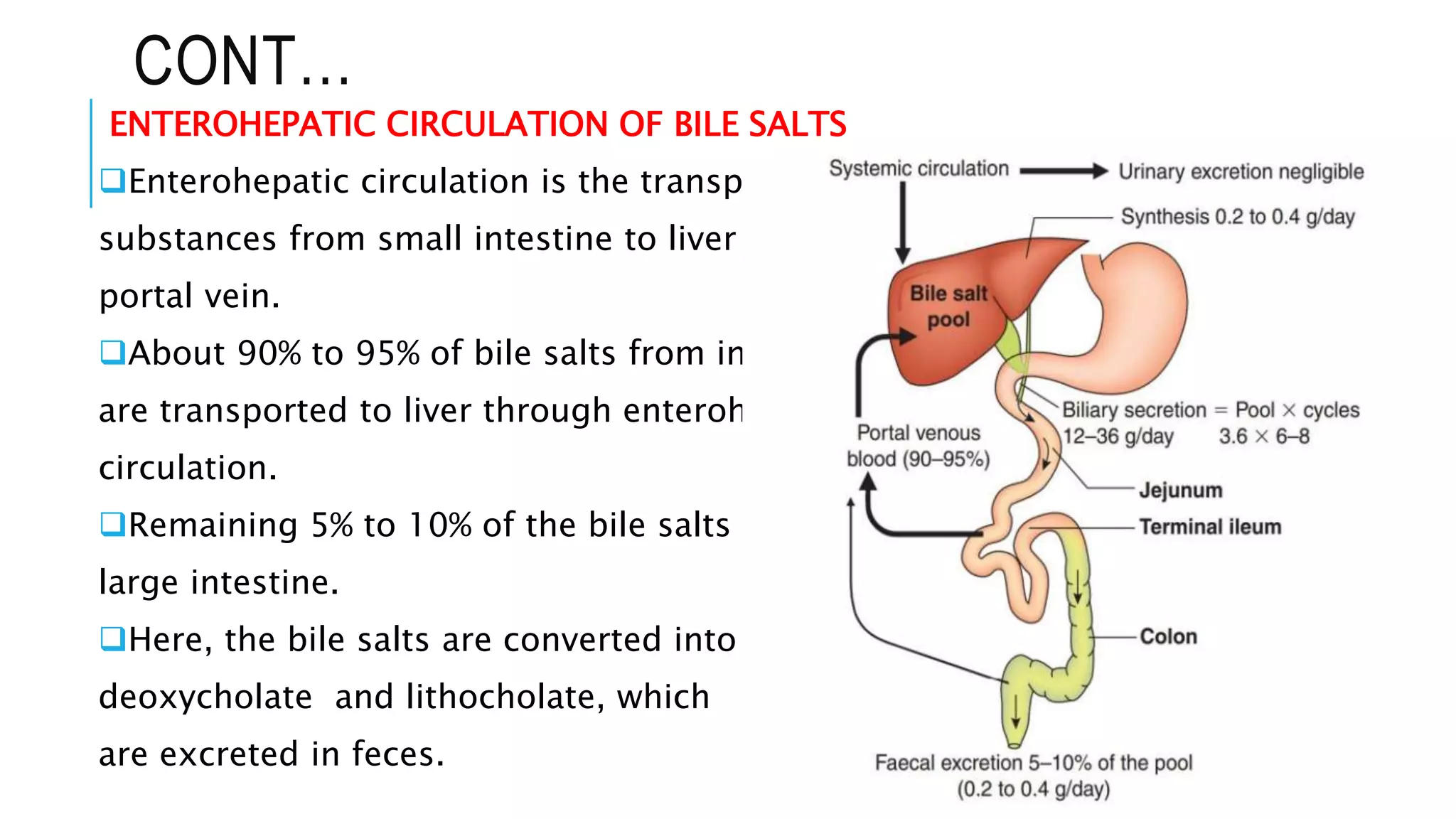
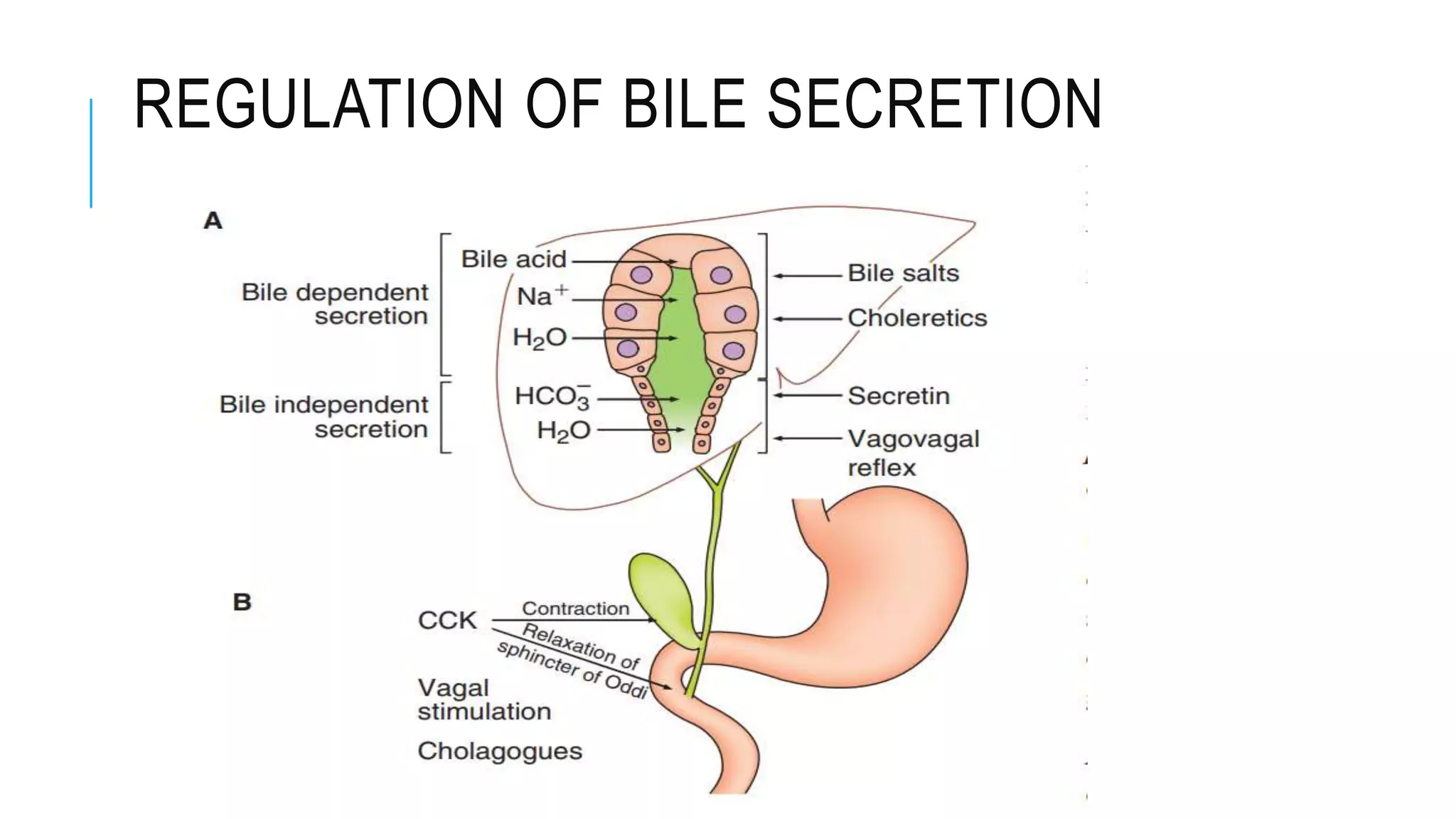
3. How bile is secreted by hepatocytes and stored/concentrated in the gallbladder before release into the small intestine.