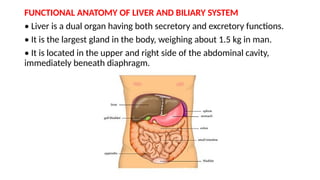
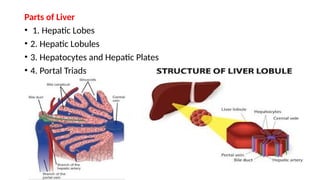
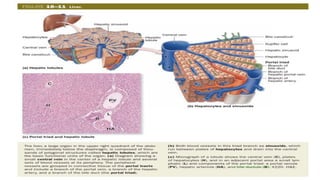
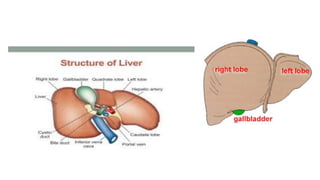
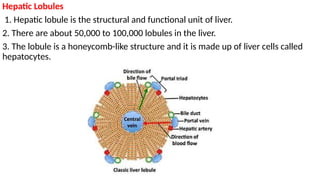
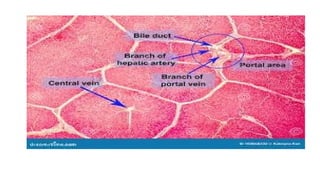
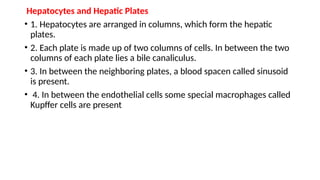
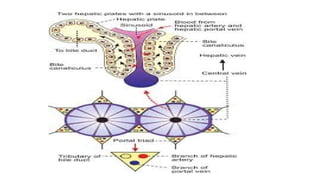
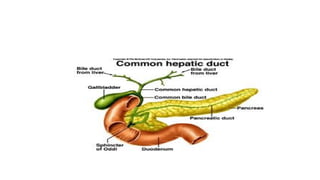
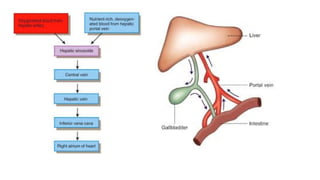
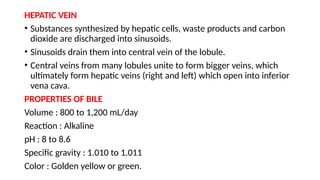
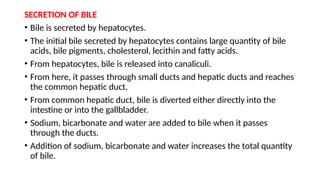
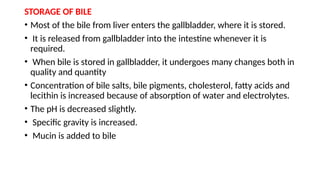
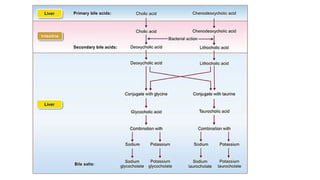
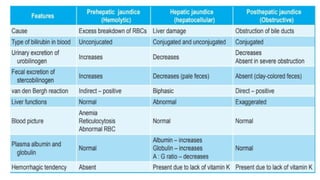
The document provides a detailed overview of the liver's anatomy and functions, highlighting its dual secretory and excretory roles, structural units like hepatic lobules, and the composition and circulation of bile. It discusses the liver's significant metabolic processes, storage capabilities, and detoxification functions, as well as common liver conditions such as jaundice, hepatitis, and cirrhosis. Additionally, it covers the gallbladder's role in bile storage and the formation of gallstones.