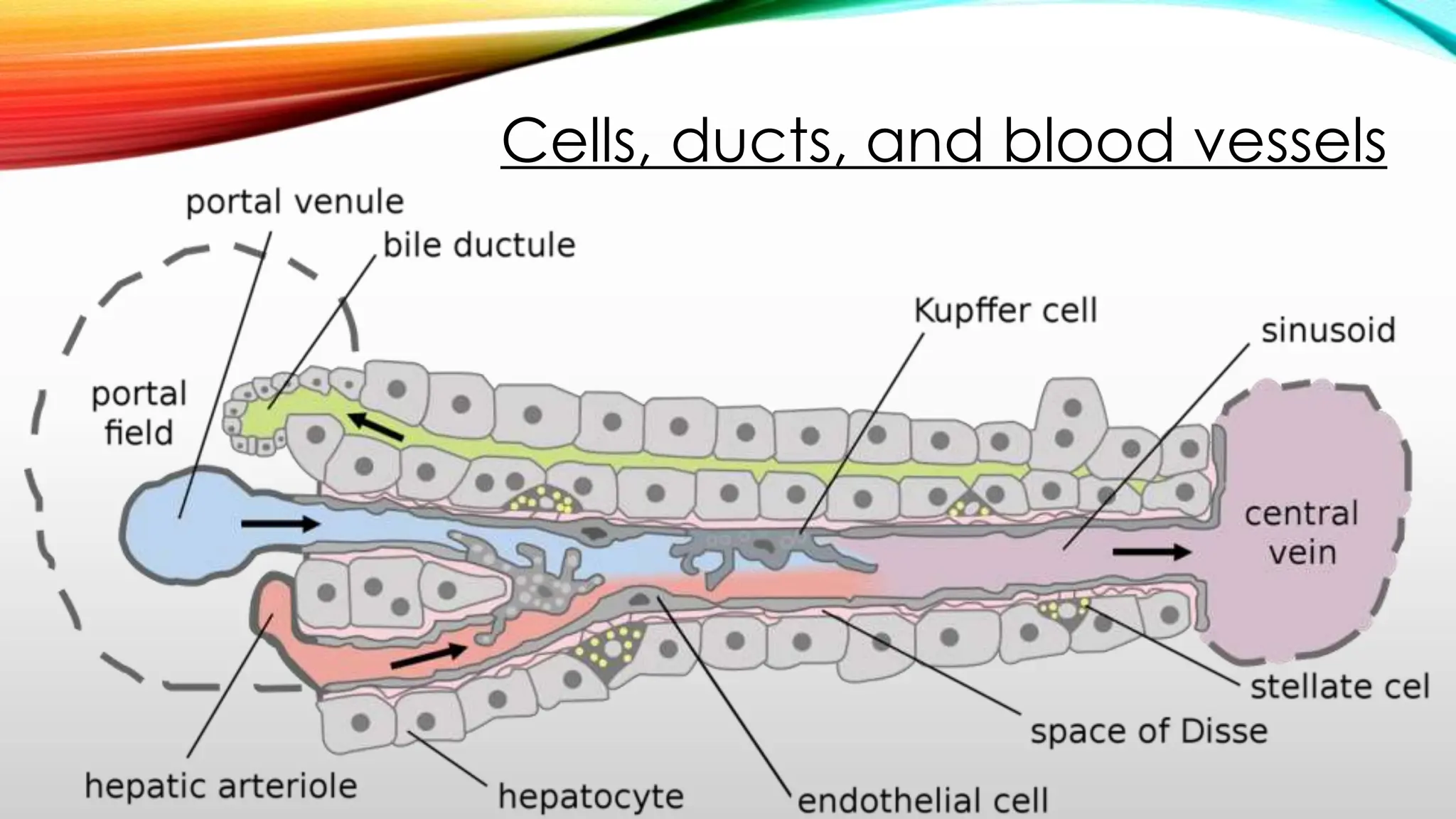
This document provides an overview of the anatomy and physiology of the liver and gallbladder, highlighting the structure, blood supply, and key functions of these organs. The liver is the largest gland in the body and is composed primarily of hepatocytes, which perform critical metabolic, secretory, and endocrine functions. Additionally, the liver plays a vital role in metabolism, detoxification, bile production, and storage of nutrients and vitamins.