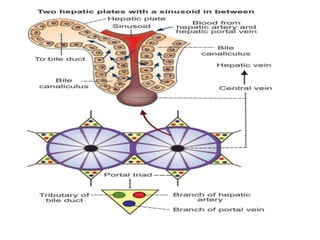
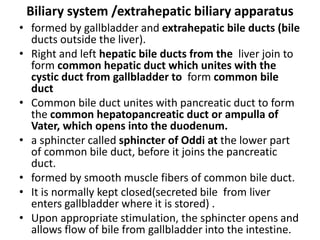
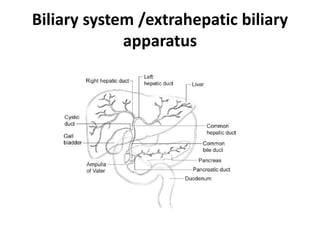
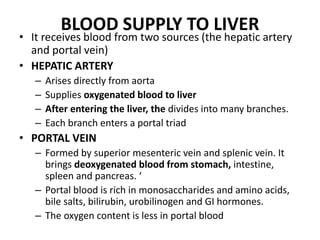
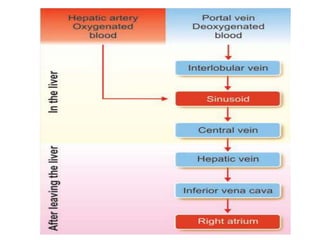
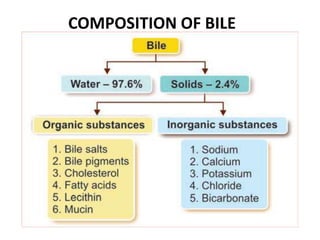
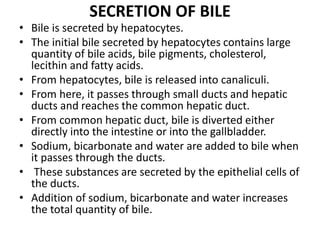
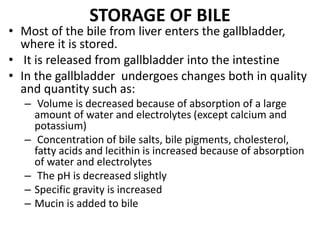
The document discusses the anatomy and physiology of the liver and gallbladder. It describes the lobular structure of the liver made up of hepatic lobules containing hepatocytes and portal triads. It also discusses the biliary system including the gallbladder and bile ducts. Key functions of the liver mentioned include metabolism, storage, synthesis of proteins and bile, and detoxification. The gallbladder stores and concentrates bile released from the liver. Jaundice and types of hepatitis are also summarized.