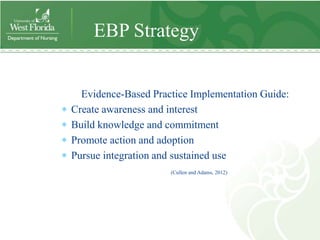
This document outlines a pilot project to develop a simulation laboratory to improve quality and safety instruction for senior nursing students. The project introduced students to simulation scenarios focusing on cardiopulmonary resuscitation. Students participated in an introductory simulation session and skills evaluation. Feedback was collected through a survey, and results suggested students felt more confident in their skills and comfortable with simulation after the sessions. The project provides a framework for evidence-based simulation implementation that can be used by other institutions.