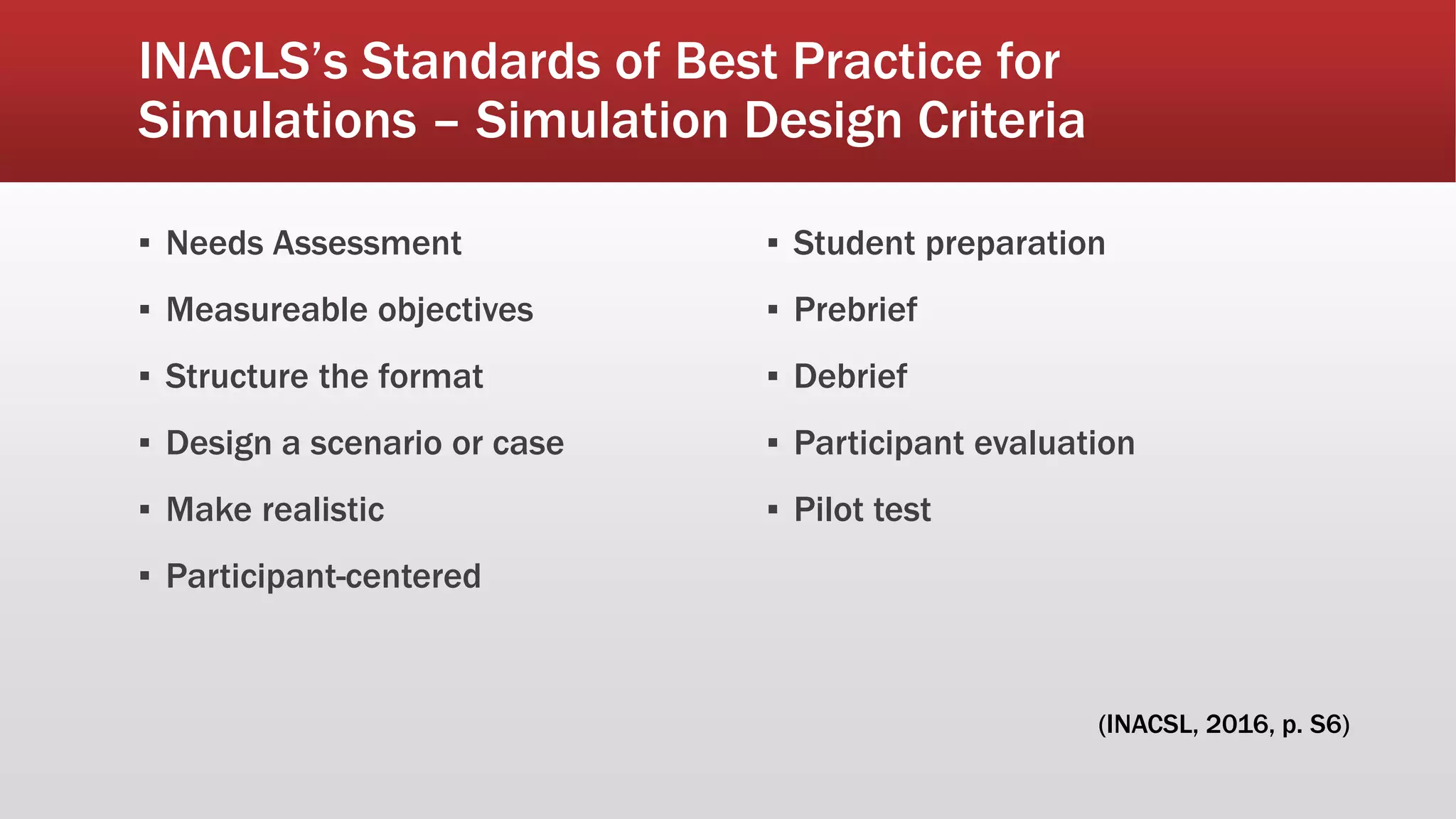
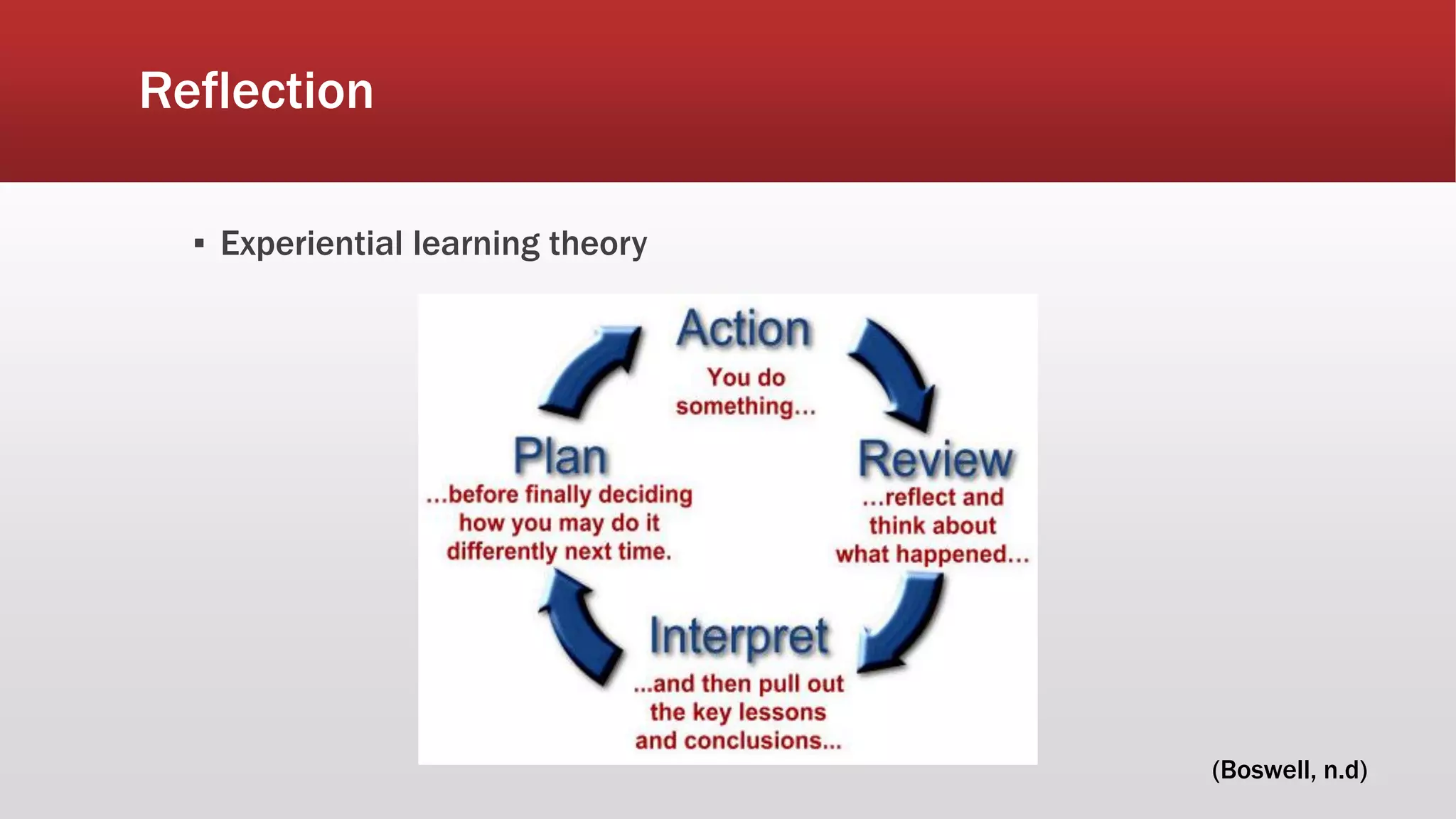
The document outlines a framework for designing systematic learning experiences in nursing simulations, based on INACSL's best practice standards. Key components include conducting a needs assessment, setting measurable objectives, effective pre-briefing and debriefing, as well as participant evaluation. The document emphasizes the importance of preparation documents, simulation realism, and the facilitation of meaningful learning through reflection.

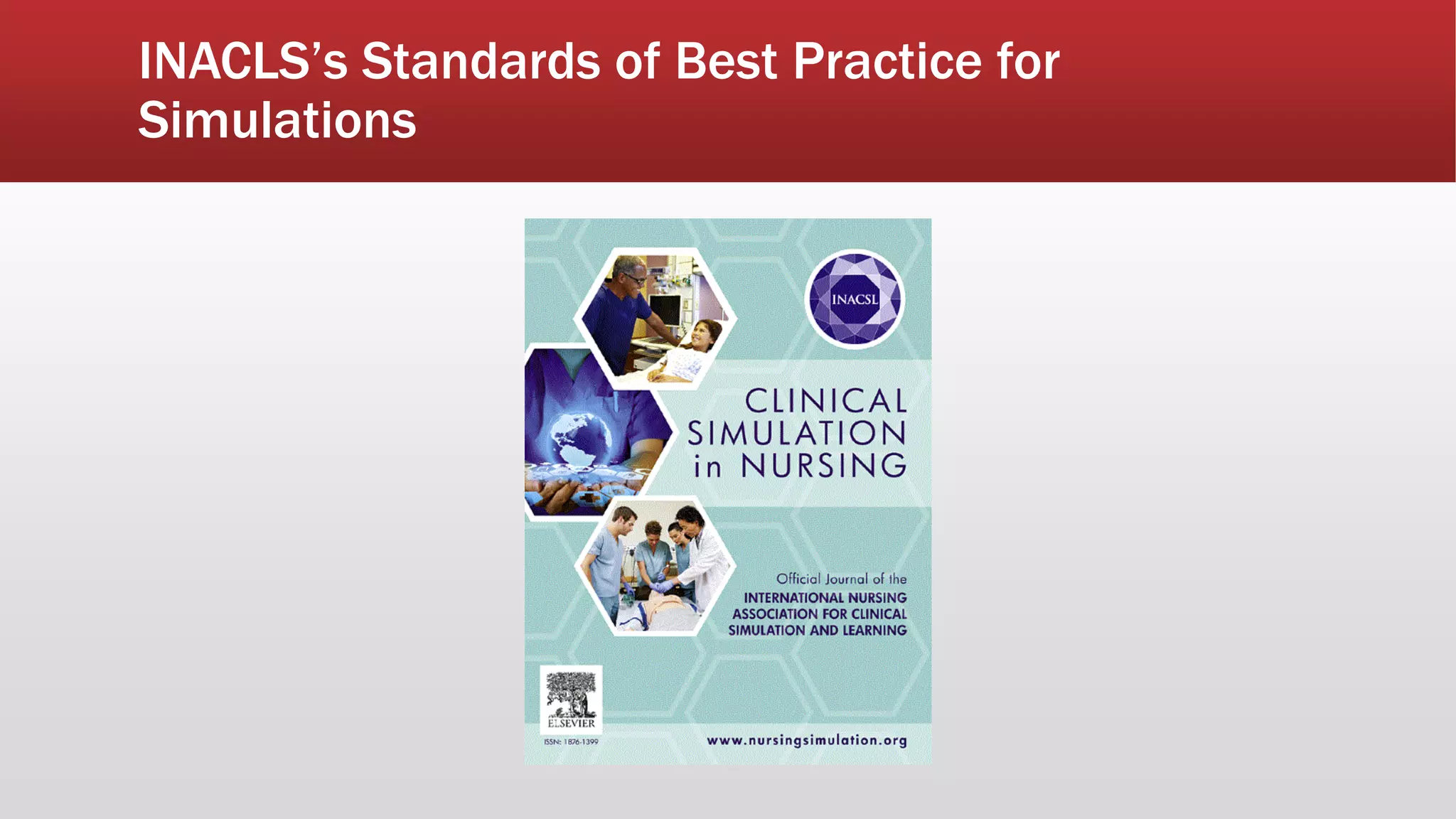
![INACLS’s Standards of Best Practice for
Simulations
Outcomes and Objective
Debriefing
Facilitation
Participant evaluation
Professional integrity
Simulation-enhanced Inter professional Education (Sim-IPE)
Simulation glossary
Simulation Design
(International Nursing Association for Clinical
Simulation and Learning [INACSL], 2016, p. S48)](https://image.slidesharecdn.com/emergingtrends-designingasystematiclearningexperienceutilizingsimulation-170523122927/75/Bailey-presentation-6-1-2017-4-2048.jpg)
![References
▪ Boswell, S. [Sam]. (n.d.). Action research [Pinterest page]. Retrieved May 12, 2017, from
https://www.pinterest.com/Sboswellhyde/action-research/?lp=true
▪ International Nursing Association for Clinical Simulation and Learning. (2016). INACSL Standards of best practice:
Simulation - Simulation design. Clinical Simulation in Nursing, 12(S), S5-S12.
http://dx.doi.org/10.1016/j.ecns.2016.09.005
▪ International Nursing Association for Clinical Simulation and Learning. (2016). INACSL Standards of best practice:
Simulation debriefing. Clinical Simulation in Nursing, 12(S), S21-S25. http://dx.doi.org/10.1016/j.ecns.2016.09.008
▪ International Nursing Association for Clinical Simulation and Learning. (2016). INACSL Standards of best practice:
Simulation facilitation. Clinical Simulation in Nursing, 12, S16-S20. http://dx.doi.org/10.1016/j.ecns.2016.09.007
▪ International Nursing Association for Clinical Simulation and Learning. (2016). INACSL Standards of best practice:
Simulation outcomes and objectives. Clinical Simulation in Nursing, 12(S), S13-S15.
http://dx.doi.org/10.1016/j.ecns.2016.09.006
▪ International Nursing Association for Clinical Simulation and Learning. (2016). INACSL Standards of best practice:
Simulation participant evaluation. Clinical Simulation in Nursing, 12(S), S26-S29.
http://dx.doi.org/10.1016/j.ecns.2016.09.009
▪ International Nursing Association for Clinical Simulation and Learning. (2016). Standards of best practice: Simulation.
Clinical Simulation in Nursing, 12(S), S48-S50. http://dx.doi.org/10.1016/j.ecns.2016.10.001](https://image.slidesharecdn.com/emergingtrends-designingasystematiclearningexperienceutilizingsimulation-170523122927/75/Bailey-presentation-6-1-2017-19-2048.jpg)