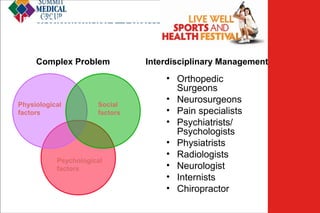
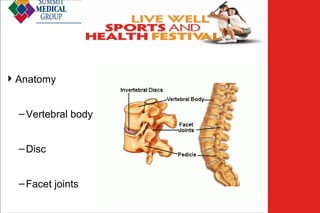
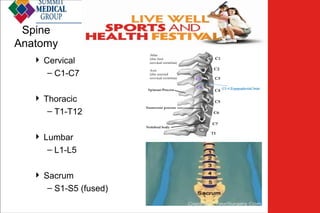
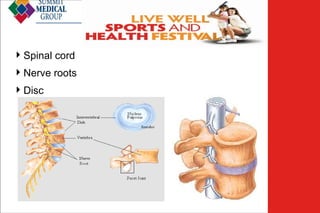
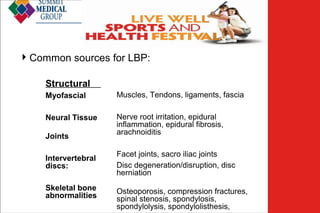
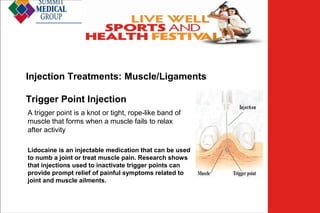
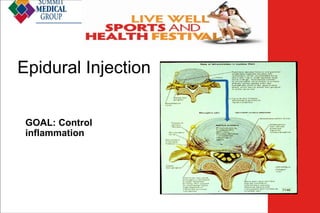
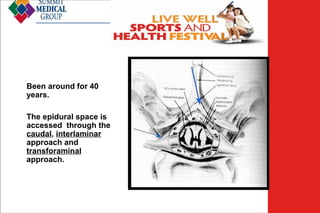
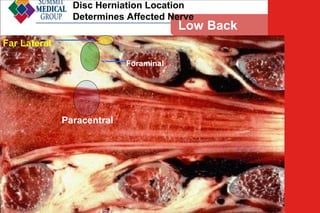
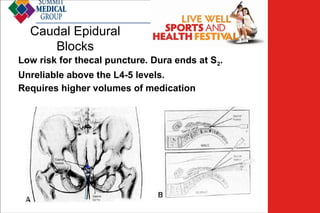
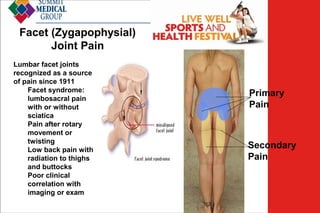
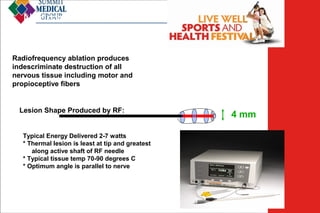
Low back pain (LBP) affects 60-90% of adults and is a leading cause of disability, with effective management requiring a comprehensive, interdisciplinary approach. Injection treatments, including trigger point injections, epidural injections, and facet joint injections, are valuable in diagnosing and alleviating symptoms of LBP. Emerging research on regenerative therapies aims to enhance healing of degenerative disc diseases, highlighting the importance of multimodal strategies for long-term management of chronic LBP.