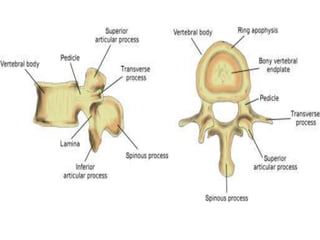
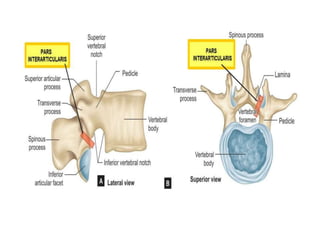
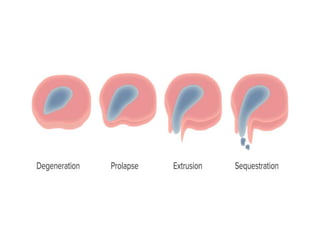
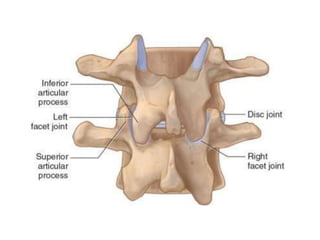
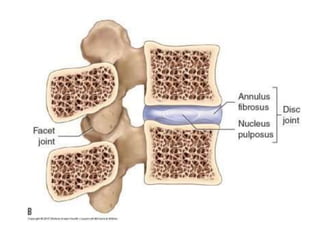
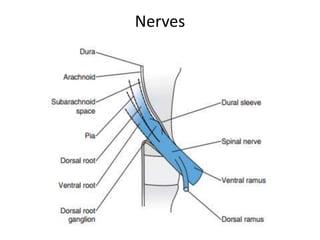
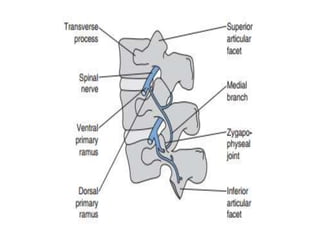
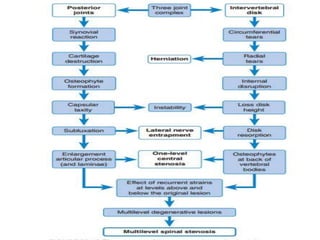
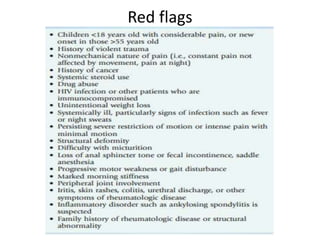
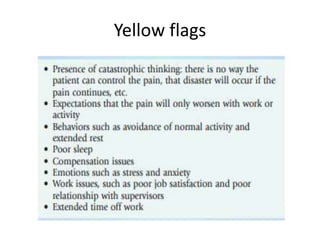
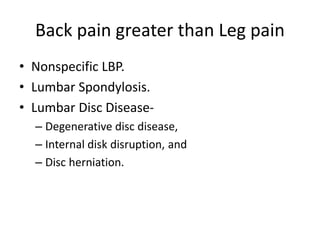
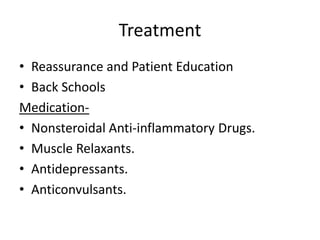
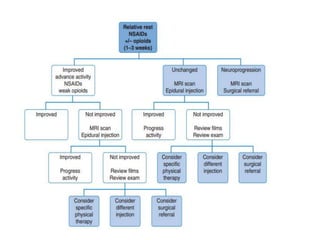
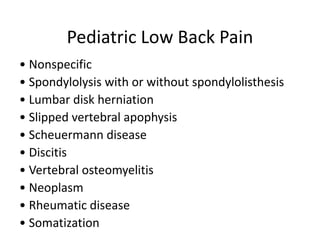
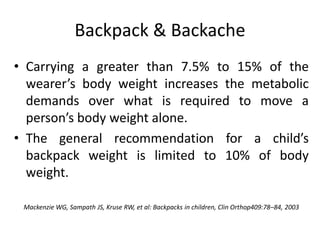
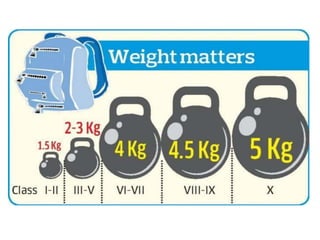
The document discusses low back pain, including its prevalence, causes, types (acute, subacute, chronic), and potential pain generators. It describes the biomechanics of the lumbar spine, including the vertebrae, intervertebral discs, zygapophyseal joints, ligaments, and muscles. Potential causes of low back pain with leg pain greater than back pain and management options are provided. Specific conditions like lumbar spinal stenosis, spondylolysis, and pregnancy-related back pain are explained. The role of ergonomics and lifestyle factors like backpack weight are also summarized.