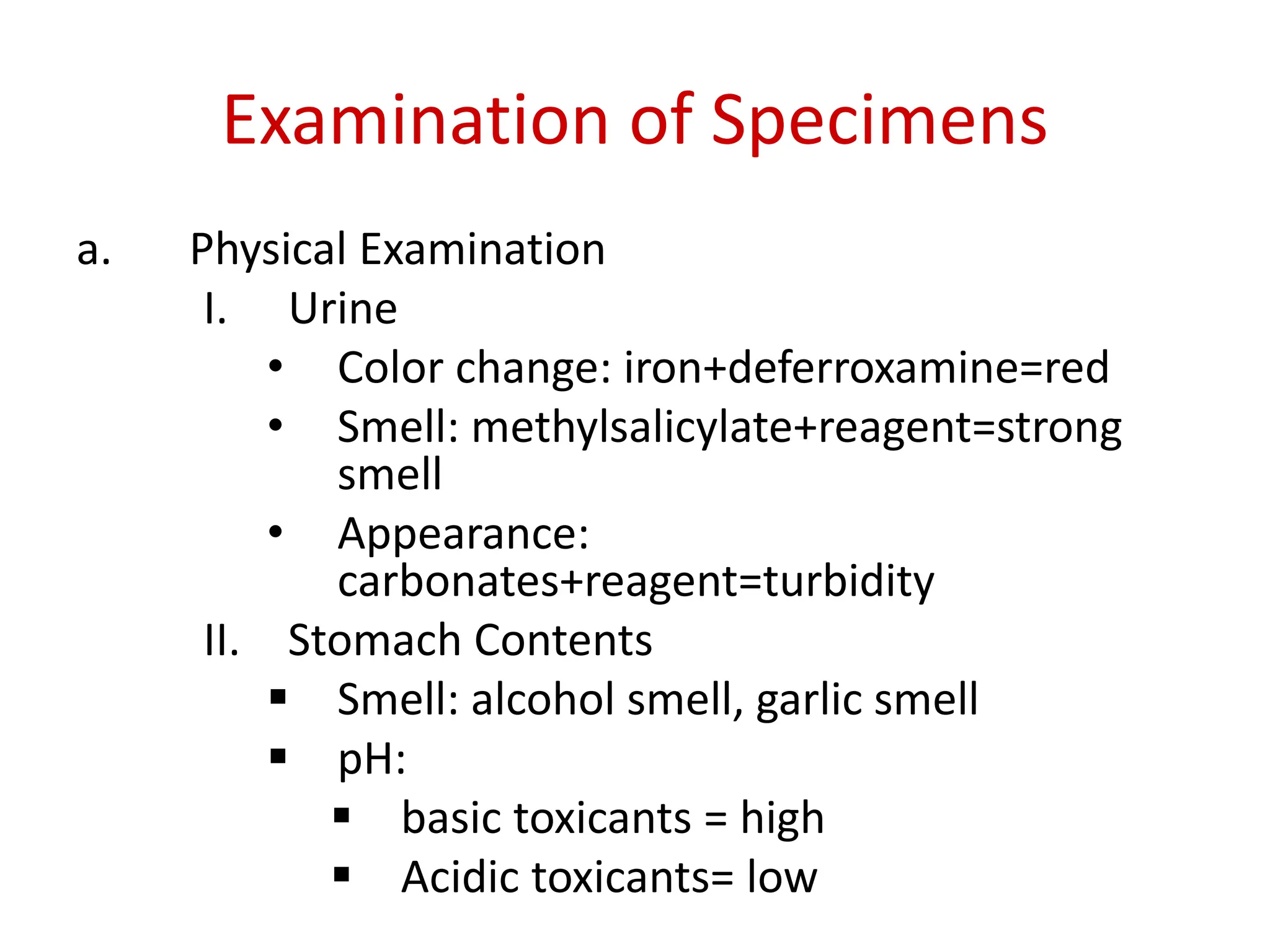
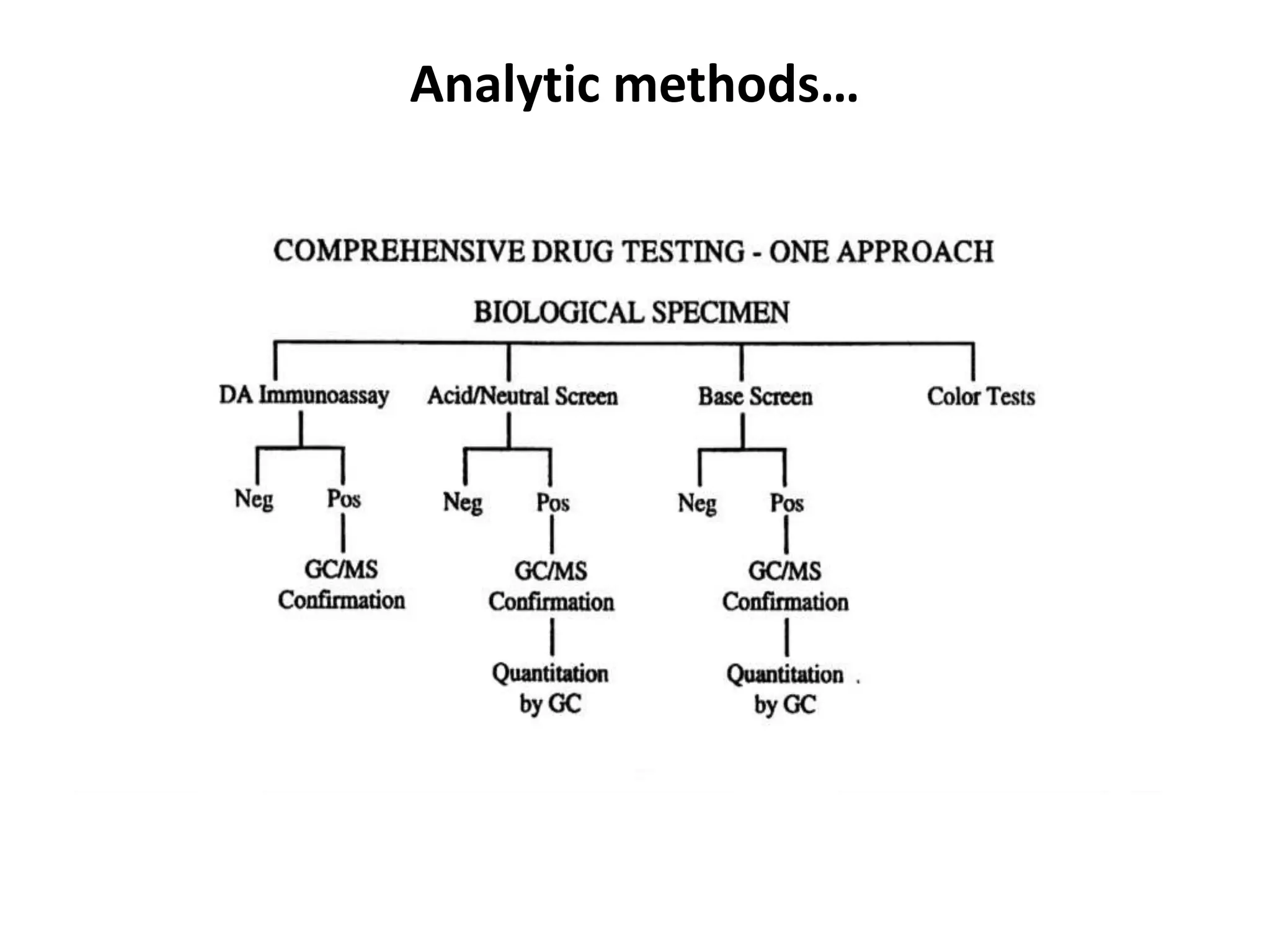
Forensic toxicology involves the analysis of biological samples to determine the presence and amount of drugs, poisons, or other chemicals in the body for legal purposes. Key aspects of forensic toxicology include postmortem toxicology analysis from autopsy samples to determine the cause of death, as well as methodology for proper collection, storage, and analysis of various sample types like blood, urine, gastric contents and more. Proper specimen collection and handling is important to ensure accurate and interpretable toxicology results.