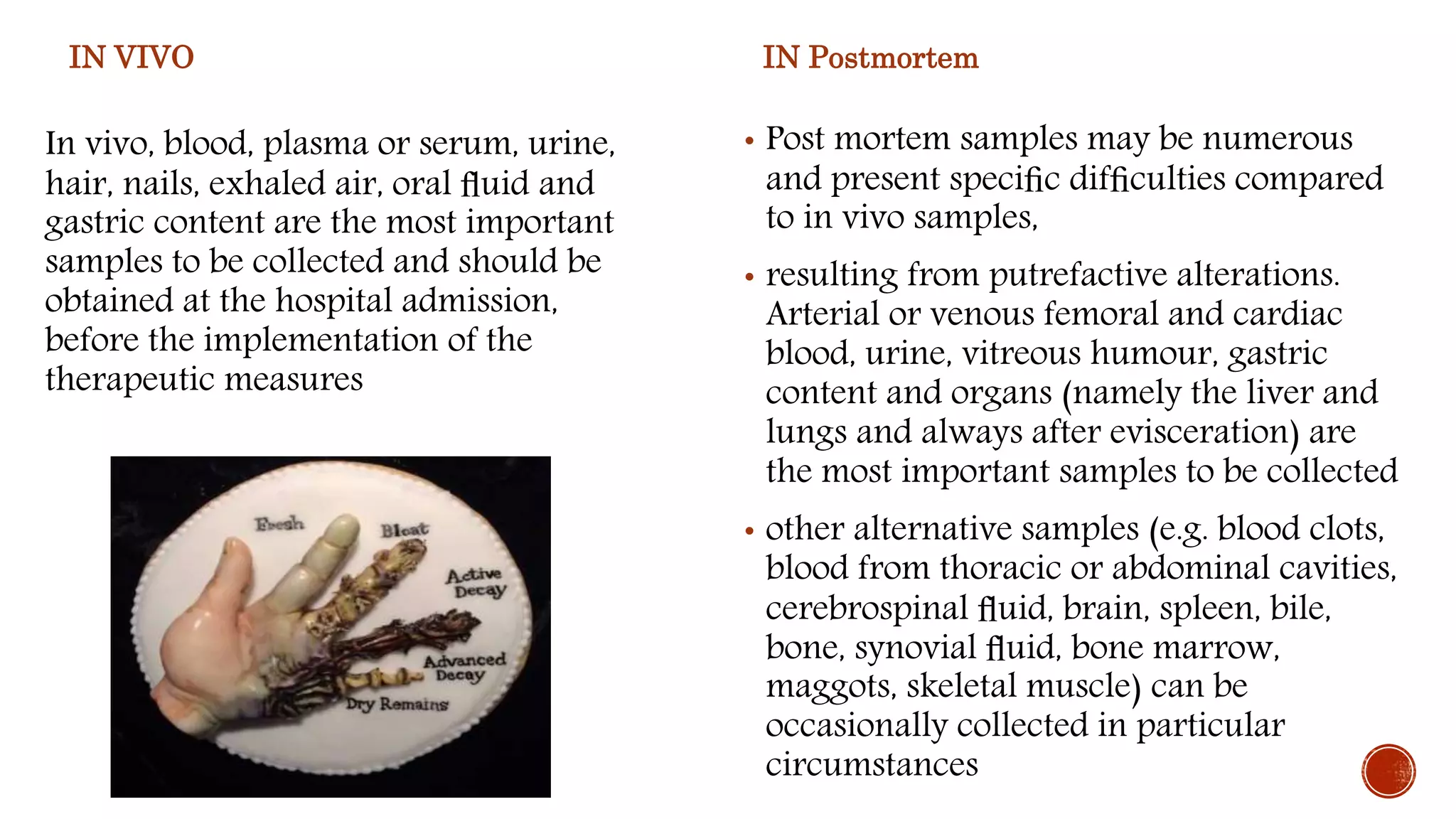
The document discusses guidelines for collecting forensic evidence from living and deceased individuals. For living individuals, blood, urine, and hair should be collected as soon as possible and labeled properly. Postmortem, blood, vitreous humor, gastric contents, and tissues like liver and lungs provide important evidence and should be collected and preserved quickly. Proper collection, labeling, storage and documentation of the chain of custody are essential for forensic analysis to identify potential toxins, drugs or other evidence of interest.