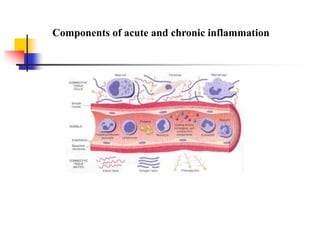
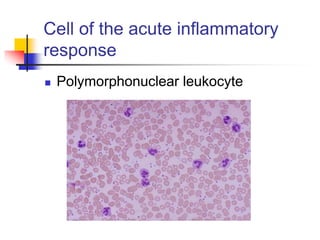
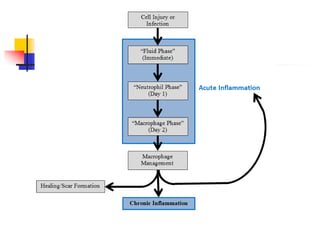
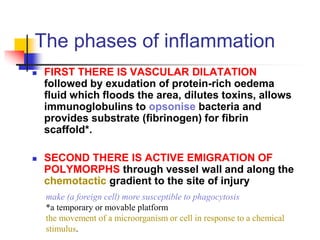
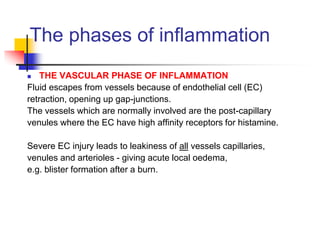
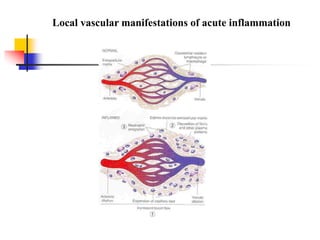
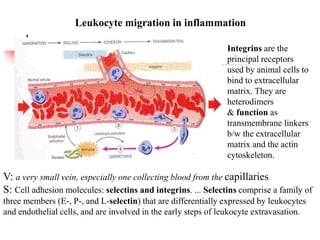
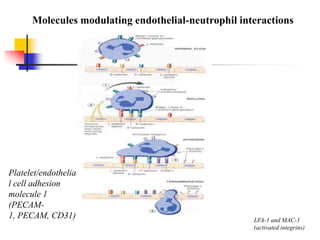
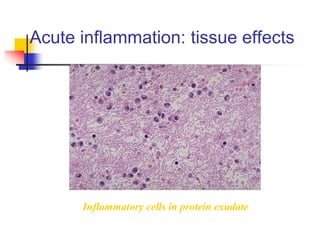
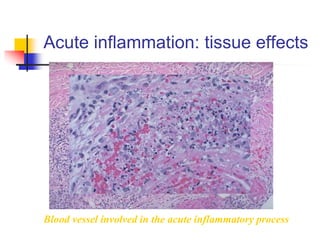
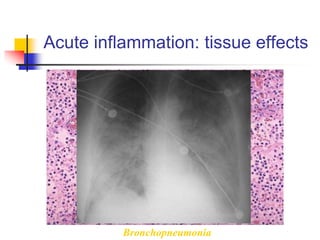
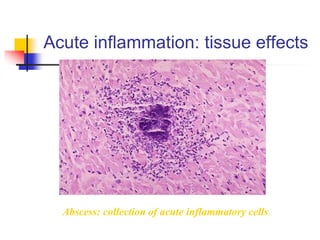
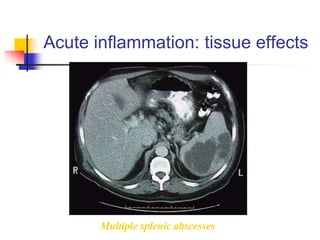
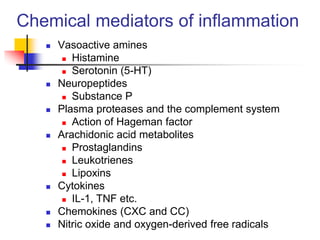
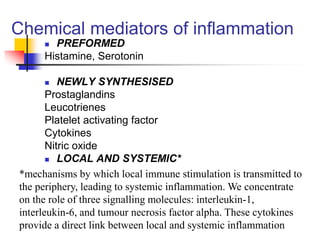
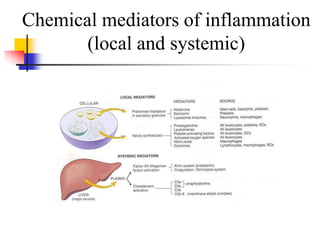
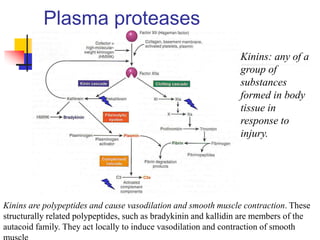
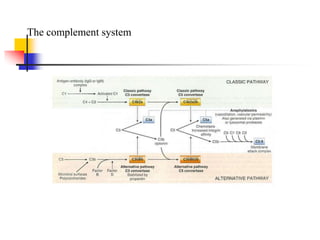
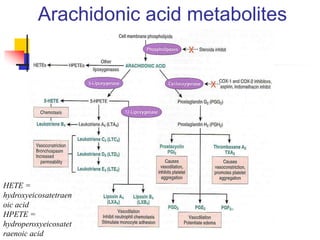
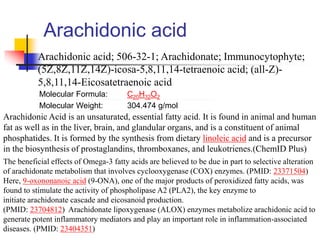
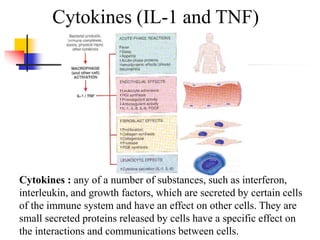
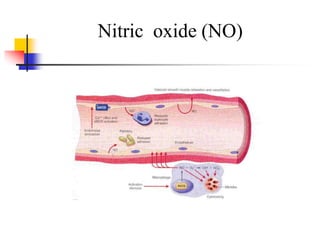
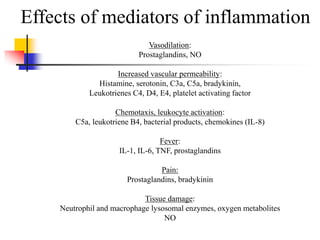
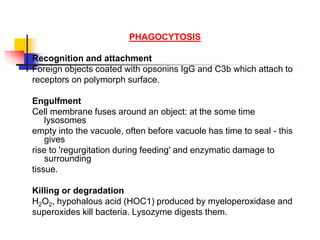
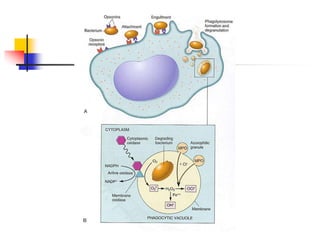
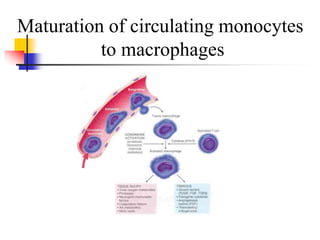
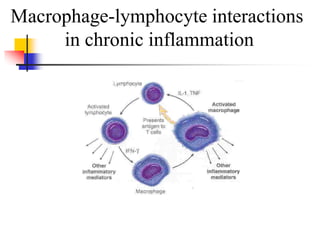
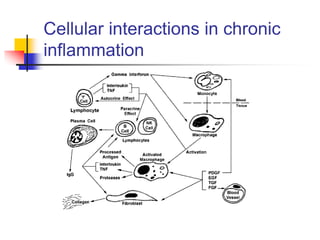
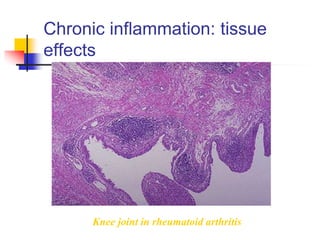
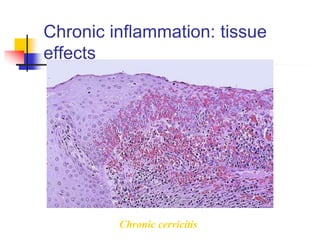
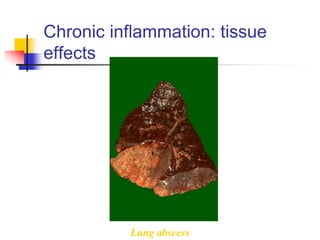
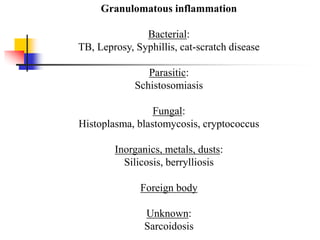
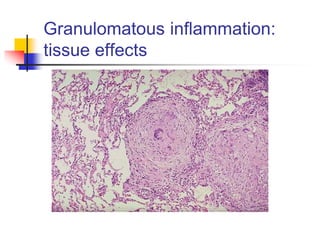
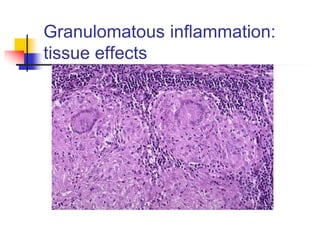
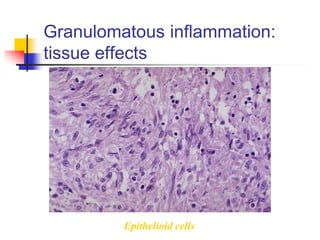
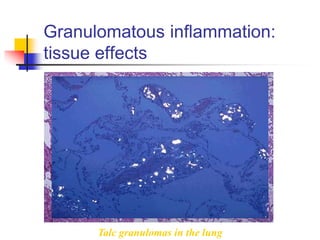
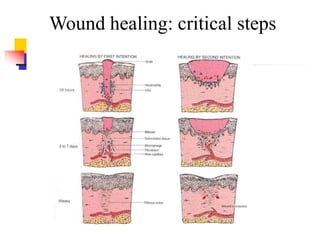
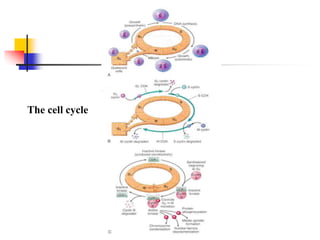
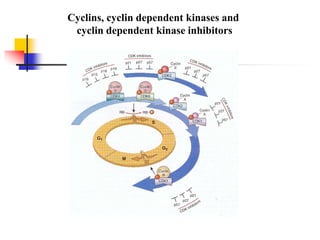
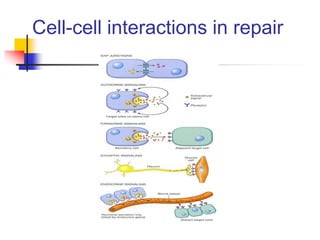
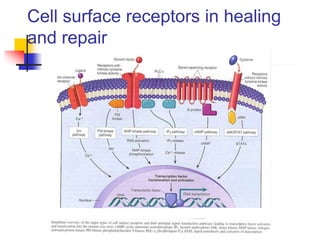
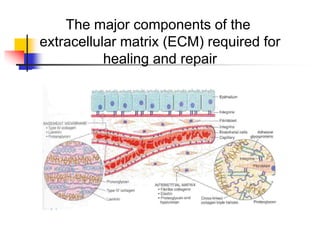
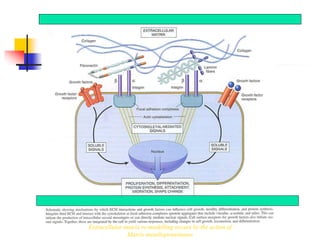
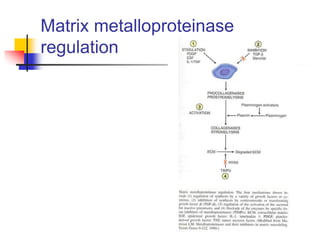
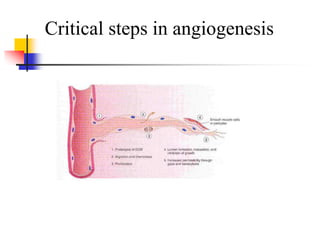
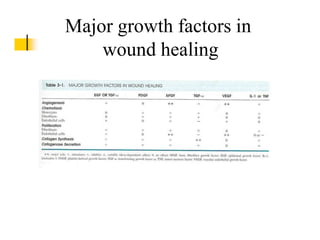
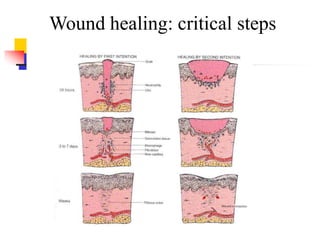
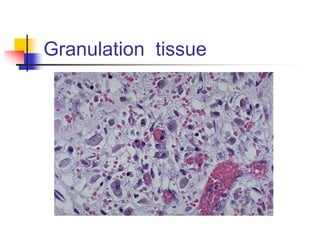
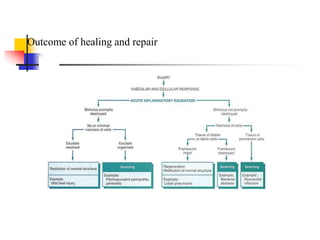
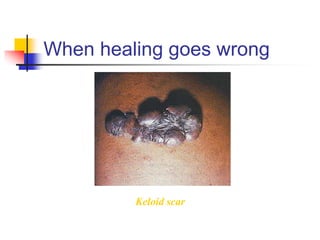
This document summarizes inflammation and the cellular responses involved. It describes inflammation as the body's protective response to injury that is interwoven with the repair process. The cardinal signs of acute inflammation are described as heat, redness, swelling, pain, and loss of function. Both acute and chronic inflammation involve vascular changes, leukocyte migration, and chemical mediators like histamine, cytokines, and arachidonic acid metabolites. Phagocytosis, granulomatous inflammation, healing, and extracellular matrix remodeling are also summarized.