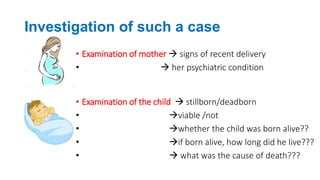
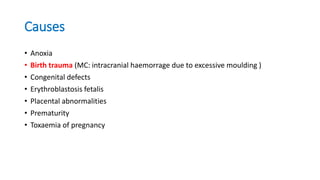
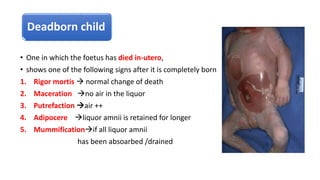
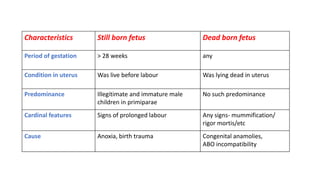
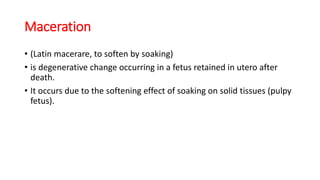
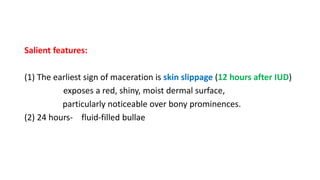
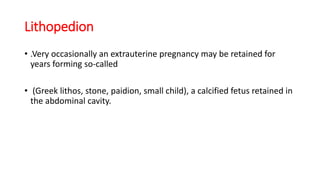
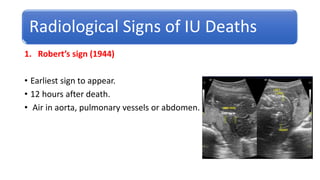
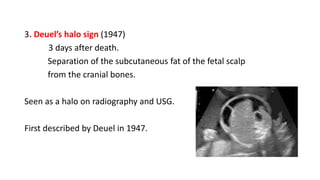
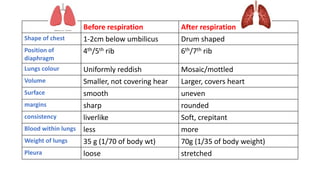
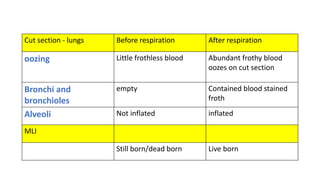
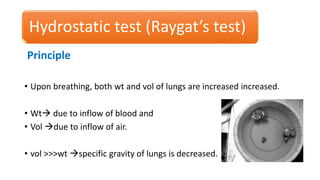
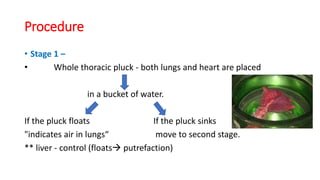
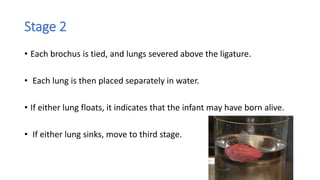
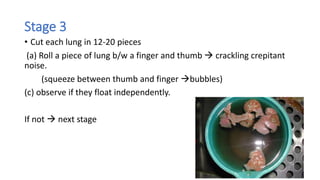
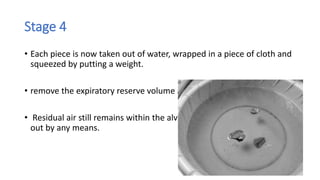
This document discusses various aspects of infanticide and determining whether a child was born alive or dead. It defines terms like infanticide, feticide, and filicide. It describes methods to investigate cases, including examining the mother and child. Signs of a live birth include changes in the lungs, stomach/intestines, and middle ear after respiration occurs. Tests like the hydrostatic test examine whether lungs float to determine if air was inhaled. The document discusses characteristics of stillborn and deadborn fetuses, maceration, and radiological signs of intrauterine death.

![2. Spalding’s sign (1922)
Appears 2 days after death.
Overlapping of fetal skull bones seen on x-ray (or ultrasound) examination.
Due to shrinkage of cerebrum after intrauterine death.
[D/d. May also be positive
(i) during or just prior to labor
(ii) scanty liquor amnii and diminished fetal vitality
(iii) microcephaly
(iv) craniostenosis]](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-18-320.jpg)

![Live birth
• [Explanation 3 of S.299, IPC].
• A child is “live born”, if any part of that child has been brought forth,
even though the child may not have breathed or been completely
born
• The Registration of Births And Deaths Act, 1969
• complete expulsion of fetus from its mother, irrespective of the
duration of pregnancy, and who after such expulsion breathes or
shows any other evidence of life](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-21-320.jpg)

![(b) Child did not respire after birth yet lungs float
• Causes:
(1) Artificial respiration - air may be found in stomach too.
(2) Putrefaction - Putrefactive gases will make the lungs float.
(3) Respiration within the womb [vagitus uterinus]-
if membranes have ruptured, but may die from natural causes
(4) Respiration within the Vagina [vagitus vaginalis] - Similar to above.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-32-320.jpg)
![Hydrostatic test is not Necessary
One is sure fetus was born dead –
(i) Born before age of viability [28 wks]
(ii) Macerated or mummified
(iii)Monster [eg anencephalic]
(iv)Bruising on lungs - indicating efforts
at artificial respiration.
One is sure fetus was born alive
(i) Stomach - contains milk
(i) Umbilical cord - has separated and
a scar has formed.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-33-320.jpg)
![(3) False +ve –
(i) Resuscitation attempts
(ii) Bacterial gas formation [putrefaction]
(4) Survival period – can be calculated:
(i) Immediate after birth – gas in stomach (upto 15 mins)
(ii) 1-2 h – Gas reaches small intestines
(iii) 5-6 h – colon
(iv) 12 h - Rectum.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-35-320.jpg)
![• (i) Regular procedure –
• Skull cap is removed and base of skull submerged in water.
• Petrous part of temporal bone [which forms roof of the middle ear] is
opened.
• If a bubble of air escapes from middle ear, the child was born alive.
• (ii) Simpler method –
• Dip ears in water. Puncture tympanic membrane"Bubble of air
escapes" Live birth.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-38-320.jpg)
![Other signs
a. Blood
• (1) Nucleated RBC"disappear in 24 h
• (2) Fetal Hb [synthesized mainly in liver]“
(i) Before birth"80-90%
(ii) 3 rd month"7-8%
(iii) 6 m"disappears completely.
b. Meconium
Completely excreted from the large intestine in 24-48 h after normal birth
May be completely excreted before birth in (a) breech presentation (b)
severe anoxia.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-39-320.jpg)


![Risk factors are
• (i) Multipara [extremely rare in primi]
• (ii) Placental abruption
• (iii) Roomy pelvis
• (iv) Small premature baby.](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-47-320.jpg)
![Criminal causes
Act of commission Act of Omission
Asphyxia
Burns
Trauma
Poisons
Abandoned child is called FONDLING
Person in-charge of the infant [mother,
father, guardian etc] can be charged u/s
302, IPC if they fail to take care of child
and allow him to die.
Failure to
(i) Clear the air passages – these may be
obstructed by amniotic fluid or mucus
(ii) Tie the cord – after it is cut. May
cause death by hemorrhage](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-52-320.jpg)

![Concealment of birth by secret disposal of dead body
before, after or during its birth,
2 y imprisonment or fine or both
[Section.318, IPC].](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-54-320.jpg)
![Injuries
• Injuries are due to direct manual violence [commonest].
(1) Tear of the frenulum
(2) Soft tissue
Pinch marks – butterfly marks
Slap marks – show as clear bruises [or as lines of petechial hgs]
resembling fingers
(3)Scalp injuries –
very characteristic. Caused by vigorous pulling on scalp hair
• Subgaleal hematoma
• Traumatic alopecia – bald patches on scalp](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-59-320.jpg)



![• (4) Eyes
(i) Black eye
(ii) Hemorrhages [Retinal, Subconjunctival, Subhyaloid, Vitreous]
(iii) Lens displacement
(iv) Retinal separation.
• (5) Skeletal injuries
(i) Skull fractures, especially in occipito-parietal area
(ii) Transverse and spiral fractures of long bones,
(twisting of arms and legs etc )](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-63-320.jpg)
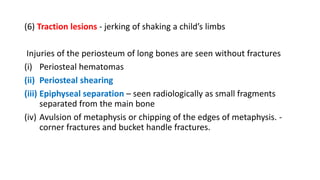
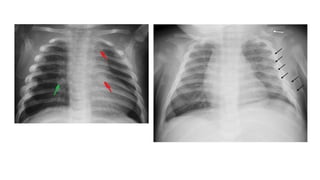
![• (7) Anteroposterior compression of chest
Fractures of ribs in midaxillary line
• (8) Side-to-side compression of chest –
along posterior angles of ribs.
After 1-2 weeks, callus forms.
X-Rays these are seen as a “string of beads” [syn, rosary bead]
paravertebral gutter [Nobbing fracture]](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-65-320.jpg)
![Visceral injuries
(1) Brain and meninges
(2) Lungs – Post-traumatic pulmonary pseudocysts [PTPPCs]
(3) Liver and spleen - Bursting injuries
(4) Hollow viscera – Ruptures
Tearing of mesentery](https://image.slidesharecdn.com/infanticide-230603143353-086b7458/85/infanticide-pptx-67-320.jpg)

