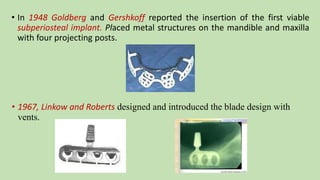
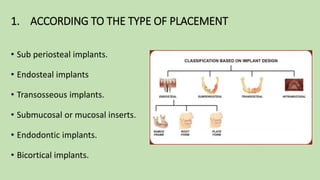
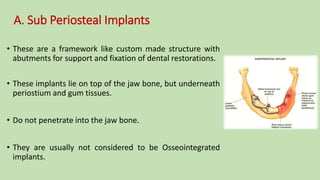
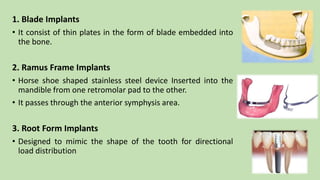
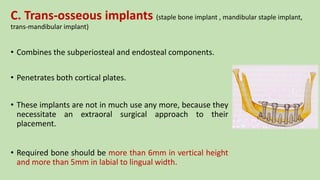
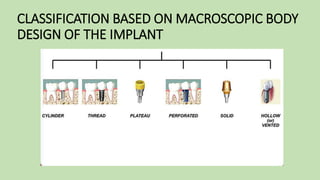
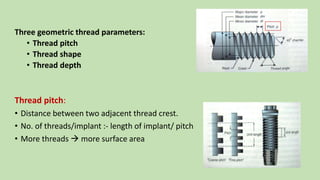
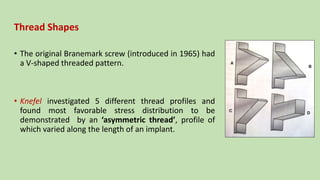
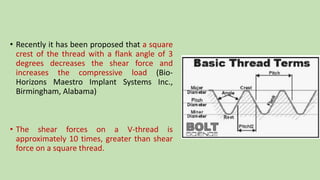
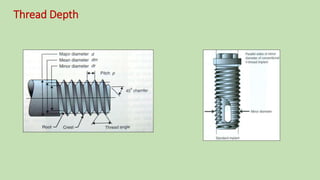
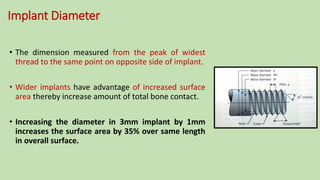
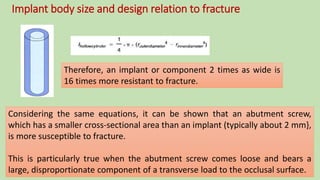
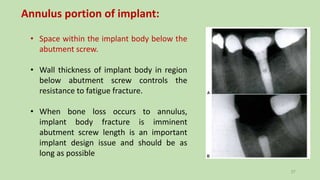
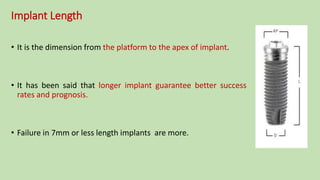
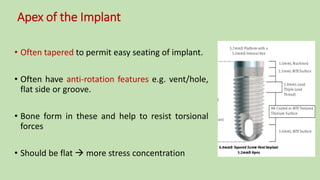
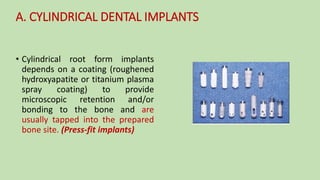
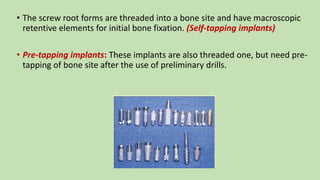
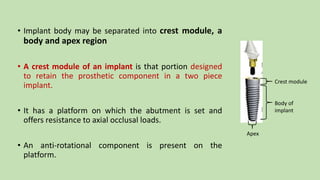
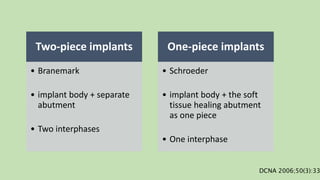
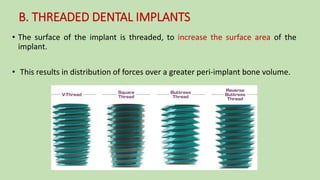
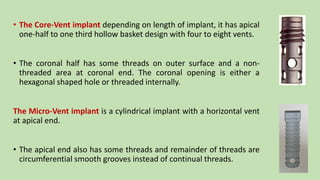
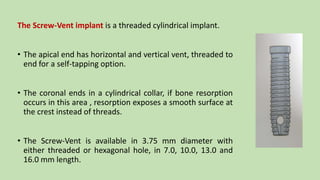
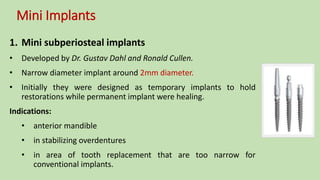
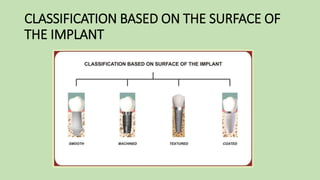
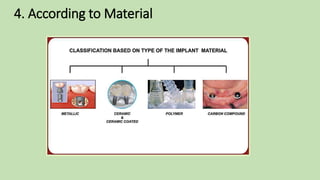
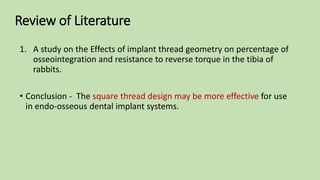
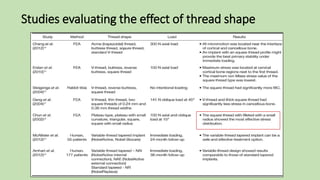
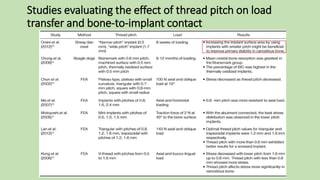
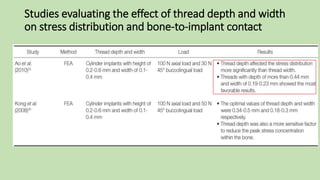
The document discusses various designs of dental implants. It describes the history of dental implants from ancient times to modern osseointegrated implants developed by Brånemark in the 1950s. It then classifies implant designs based on type of placement (e.g. endosteal, subperiosteal), macroscopic body design (e.g. cylindrical, threaded), and components (e.g. crest module, body, apex). Key design considerations discussed include thread pitch, shape and depth, implant diameter and length, and one-piece versus two-piece designs.