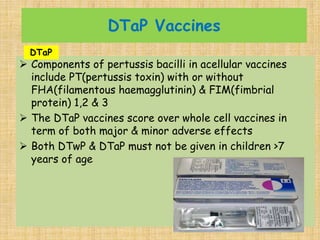
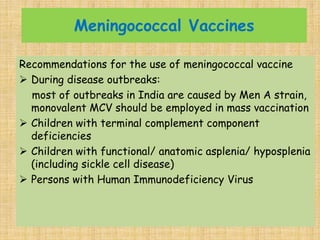
The document discusses various vaccines that are part of national immunization schedules. It describes the different types of vaccines including live attenuated, killed/inactivated, toxoid, conjugate and subunit vaccines. It provides details about vaccines for diseases like BCG, polio, diphtheria, pertussis, tetanus, measles, mumps, rubella, Hib, hepatitis B, typhoid, varicella, rotavirus and pneumococcus. It discusses the appropriate ages, doses, routes of administration, storage requirements and schedules for these vaccines. It also provides guidance on vaccination of high-risk groups and management of infants born to hepatitis B positive mothers.