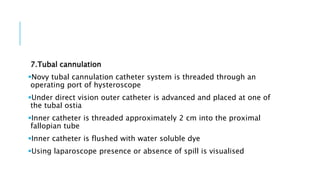
This document provides information about hysteroscopies, including what they are, the equipment used, procedures, indications, and complications.
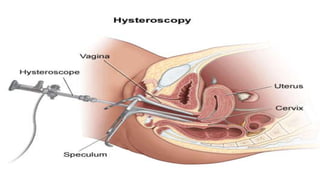
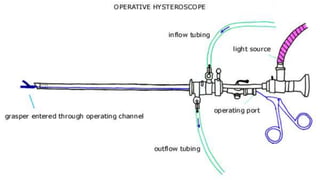
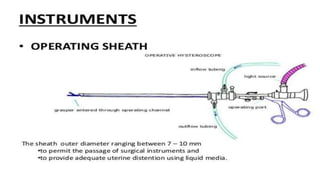
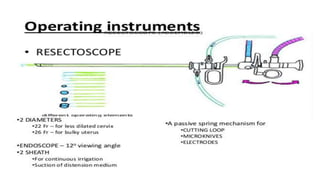
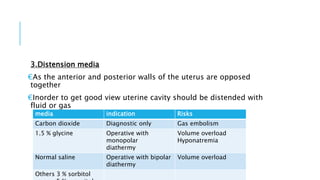
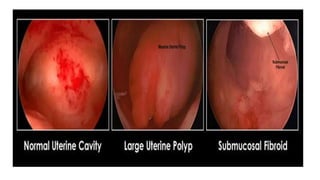
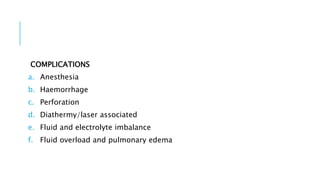
Hysteroscopies allow direct visual inspection of the cervical canal and uterine cavity and can be used for both diagnostic and therapeutic purposes. Equipment includes rigid or flexible hysteroscopes connected to a light source, camera, and monitor. Distension media like carbon dioxide, glycine, or saline is used to distend the uterine cavity during the procedure. Diagnostic hysteroscopies are used to evaluate conditions like abnormal uterine bleeding or infertility while operative hysteroscopies can be used to remove polyps, fibroids, or adhesions. Potential complications include issues from anesthesia, bleeding,