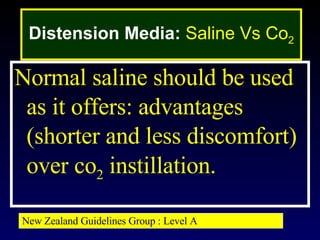
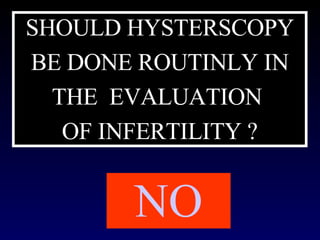
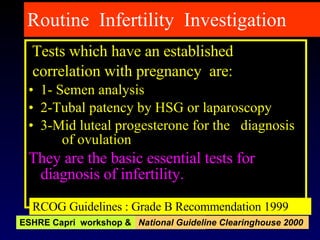
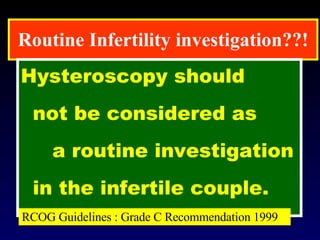
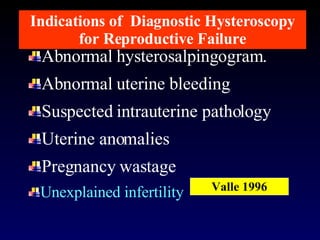
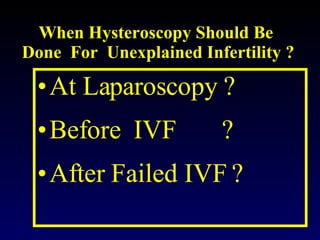
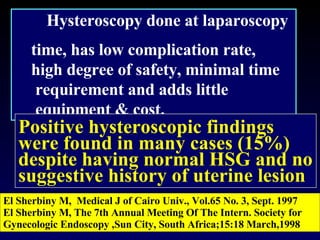
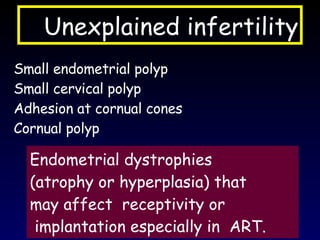
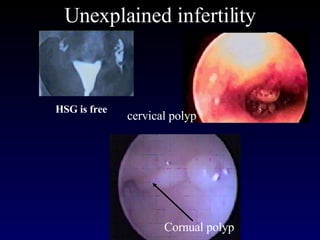
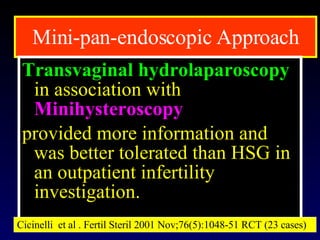
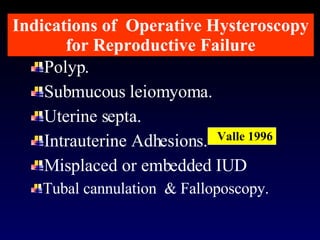
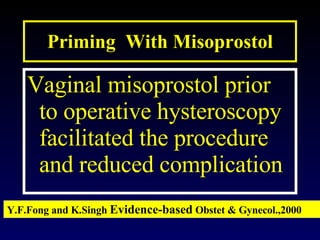
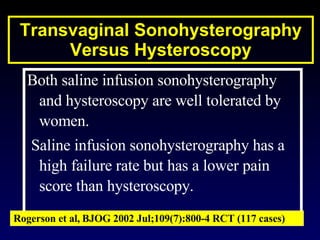
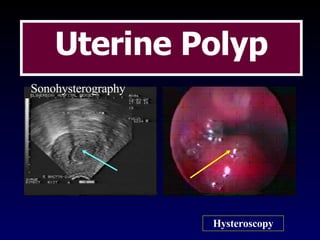
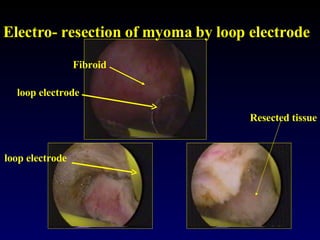
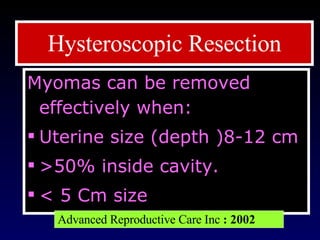
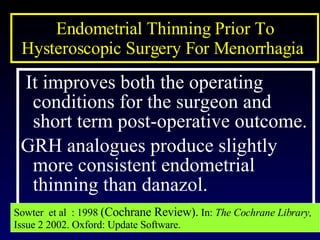
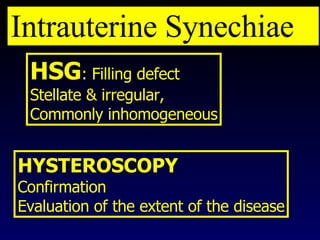
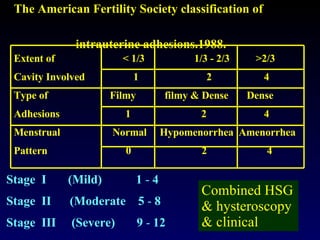
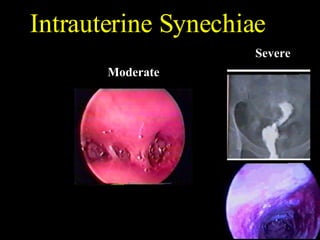
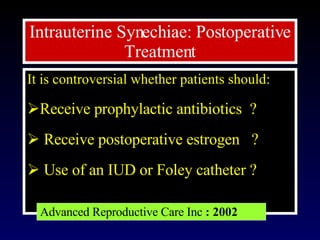
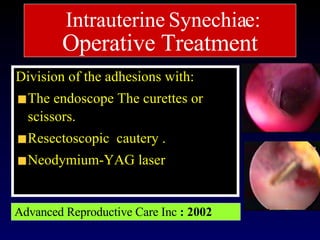
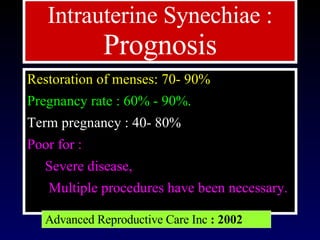
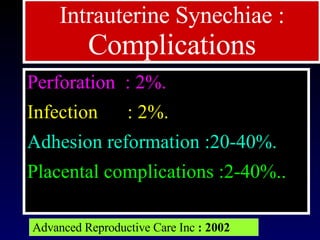
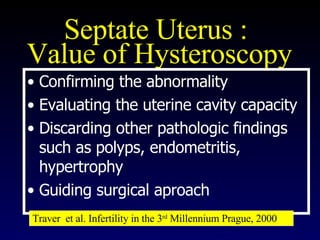
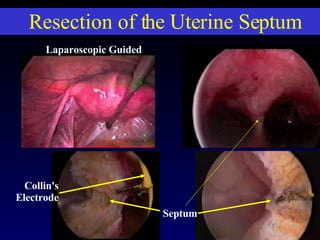
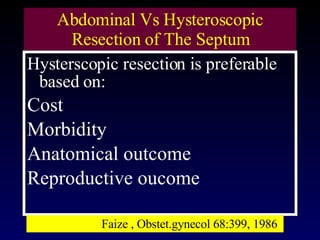
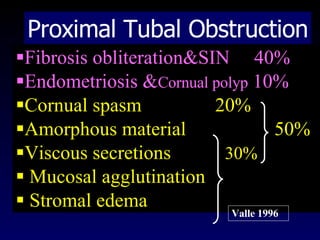
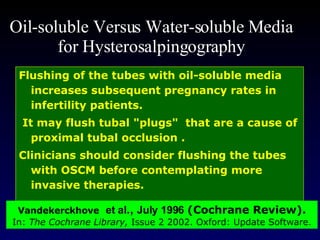
The document discusses the use of hysteroscopy in evaluating and treating infertility. It provides evidence-based guidelines on when hysteroscopy is recommended and not recommended in infertility workup. It also reviews evidence on techniques for diagnostic and operative hysteroscopy, including indications, preparation, distension media, findings, and treatment of various intrauterine issues like polyps, fibroids, adhesions that may cause infertility. Complications are also discussed.