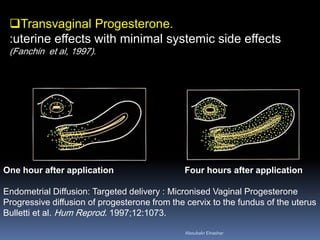
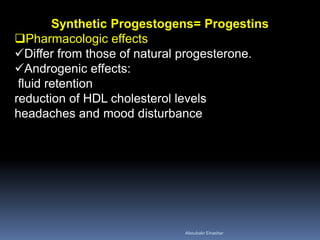
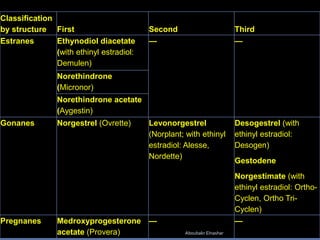
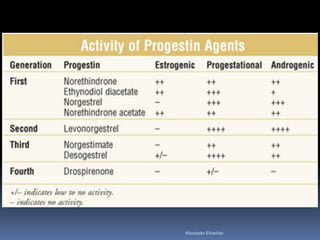
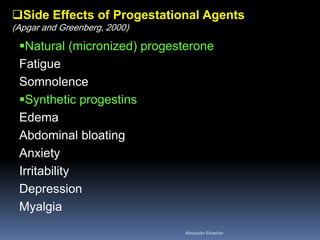
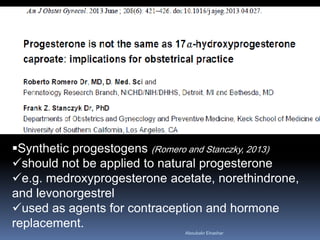
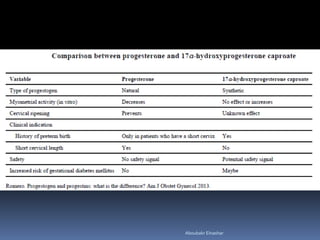
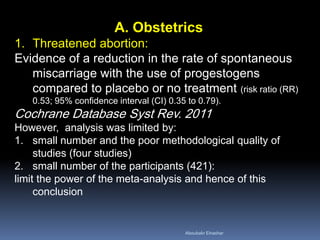
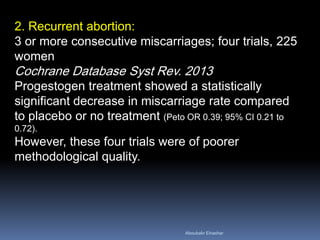
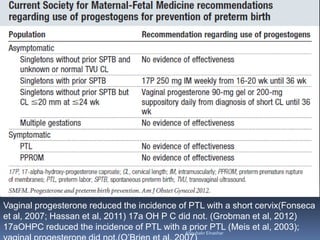
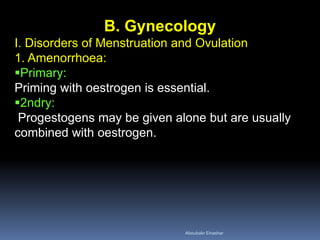
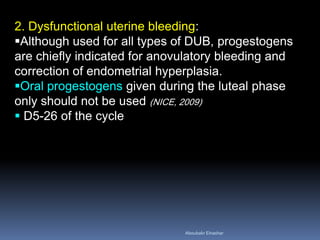
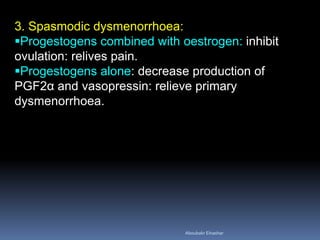
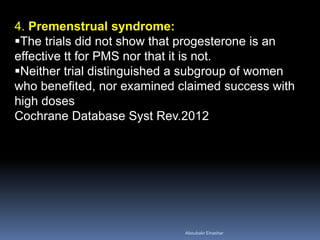
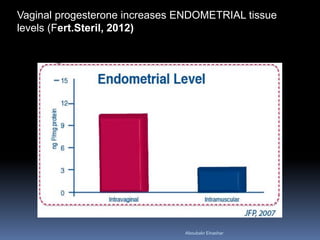
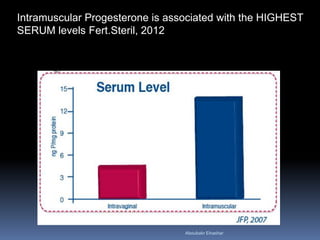
The document discusses progestogens, which include progesterone and synthetic progestins. Progesterone is secreted naturally, while progestins have progesterone-like effects. Both are used for obstetric and gynecologic purposes. Therapeutically, progestogens are used to support early pregnancy, treat menstrual disorders, provide luteal phase support in assisted reproduction, and relieve symptoms of conditions like endometriosis. While generally effective, studies on uses like threatened miscarriage and preterm labor have been limited by small sample sizes. Natural progesterone generally has fewer side effects than progestins. The document examines various progestogen types and routes of administration.