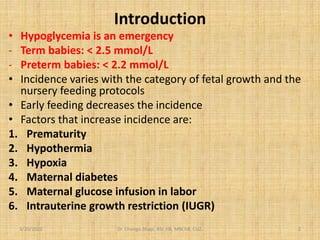
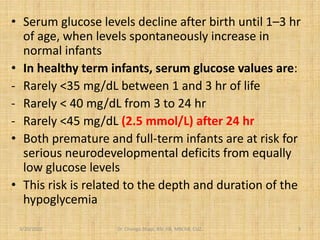
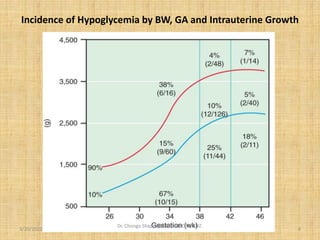
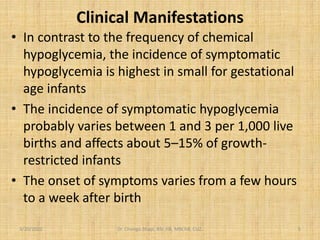
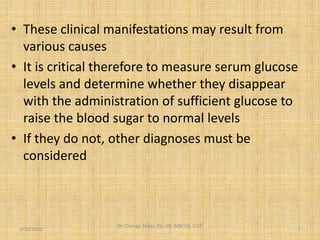
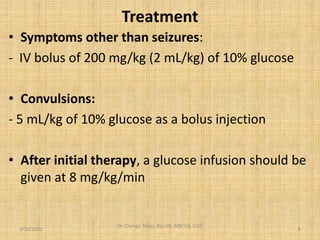
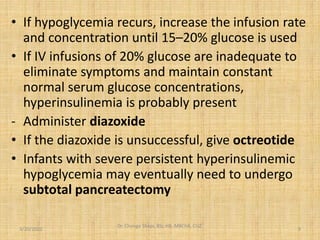
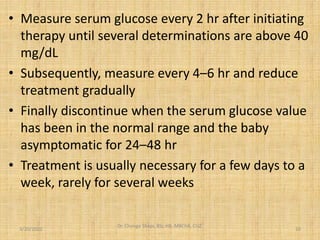
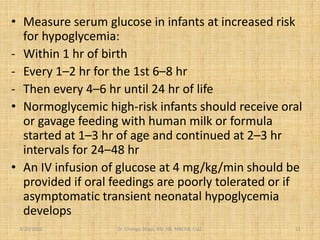
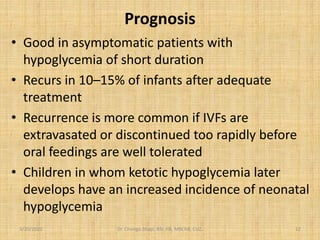
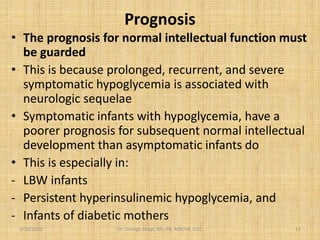
Hypoglycemia in neonates can be a critical emergency, particularly affecting preterm and small for gestational age infants, with a variety of symptoms including jitteriness and lethargy. Treatment typically involves glucose administration, with monitoring and adjustments as necessary, particularly for infants at high risk. Prognosis for normal intellectual function is cautious, particularly for those with recurrent or severe hypoglycemia, as it can lead to neurological issues.