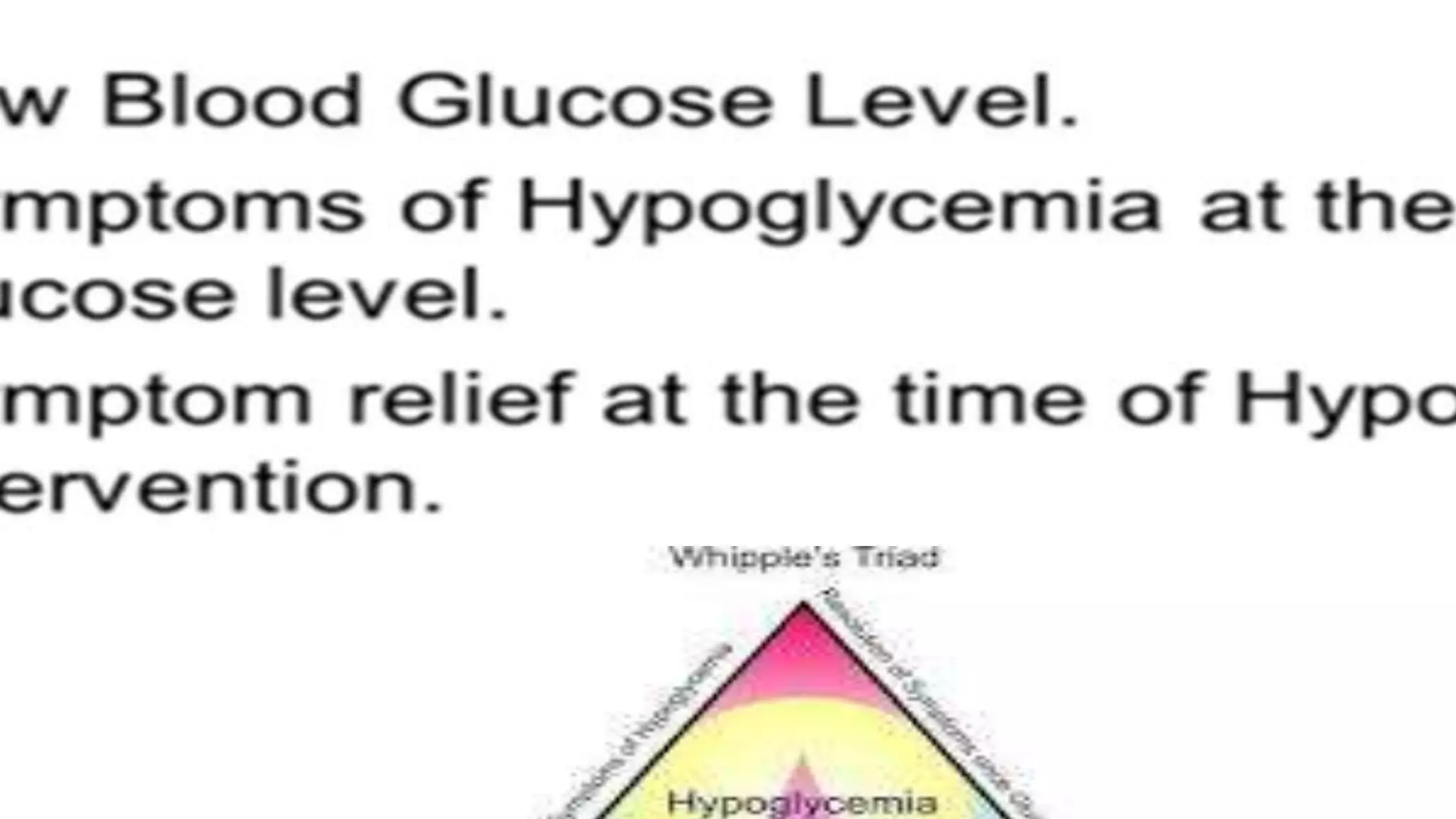
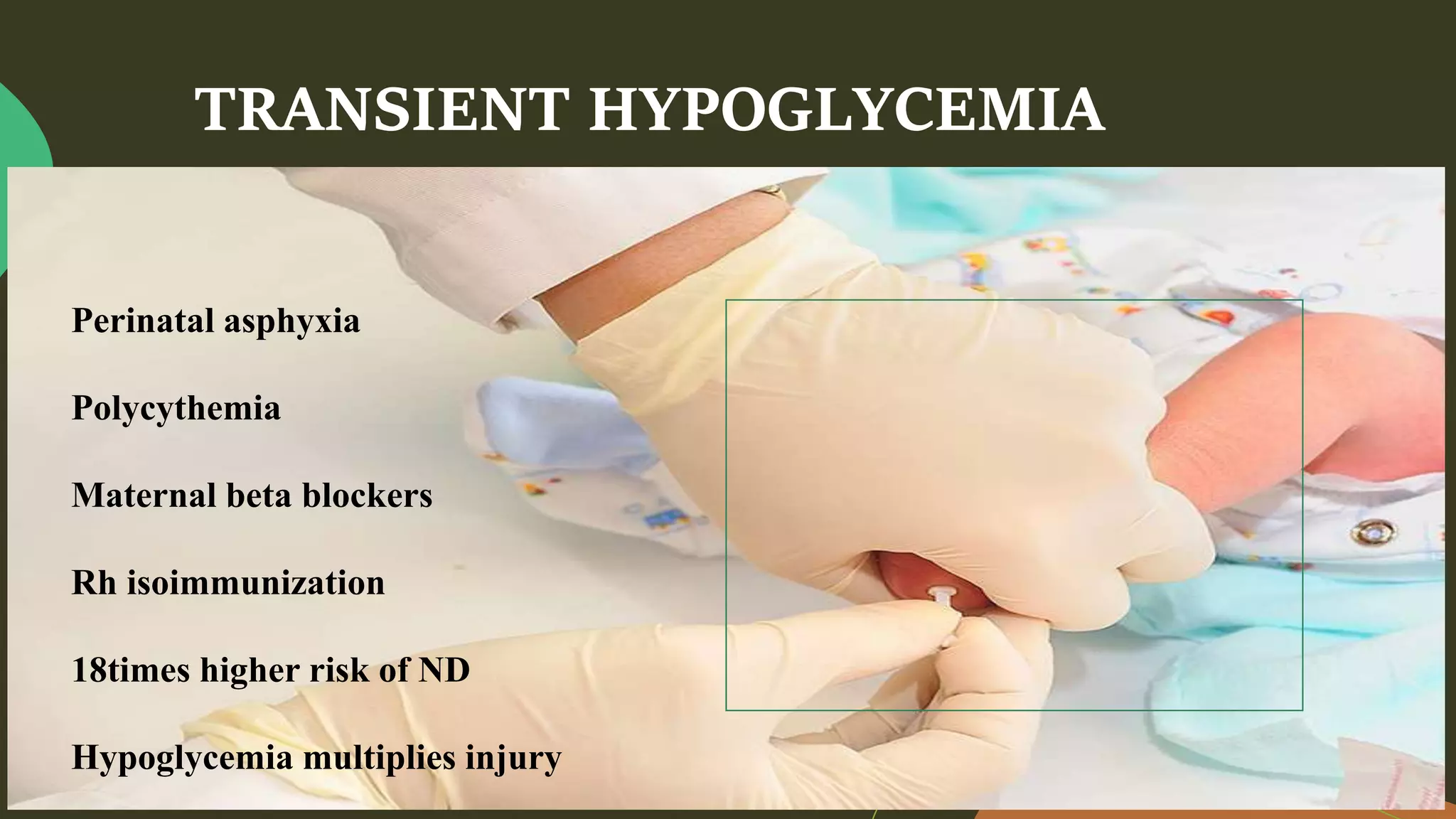
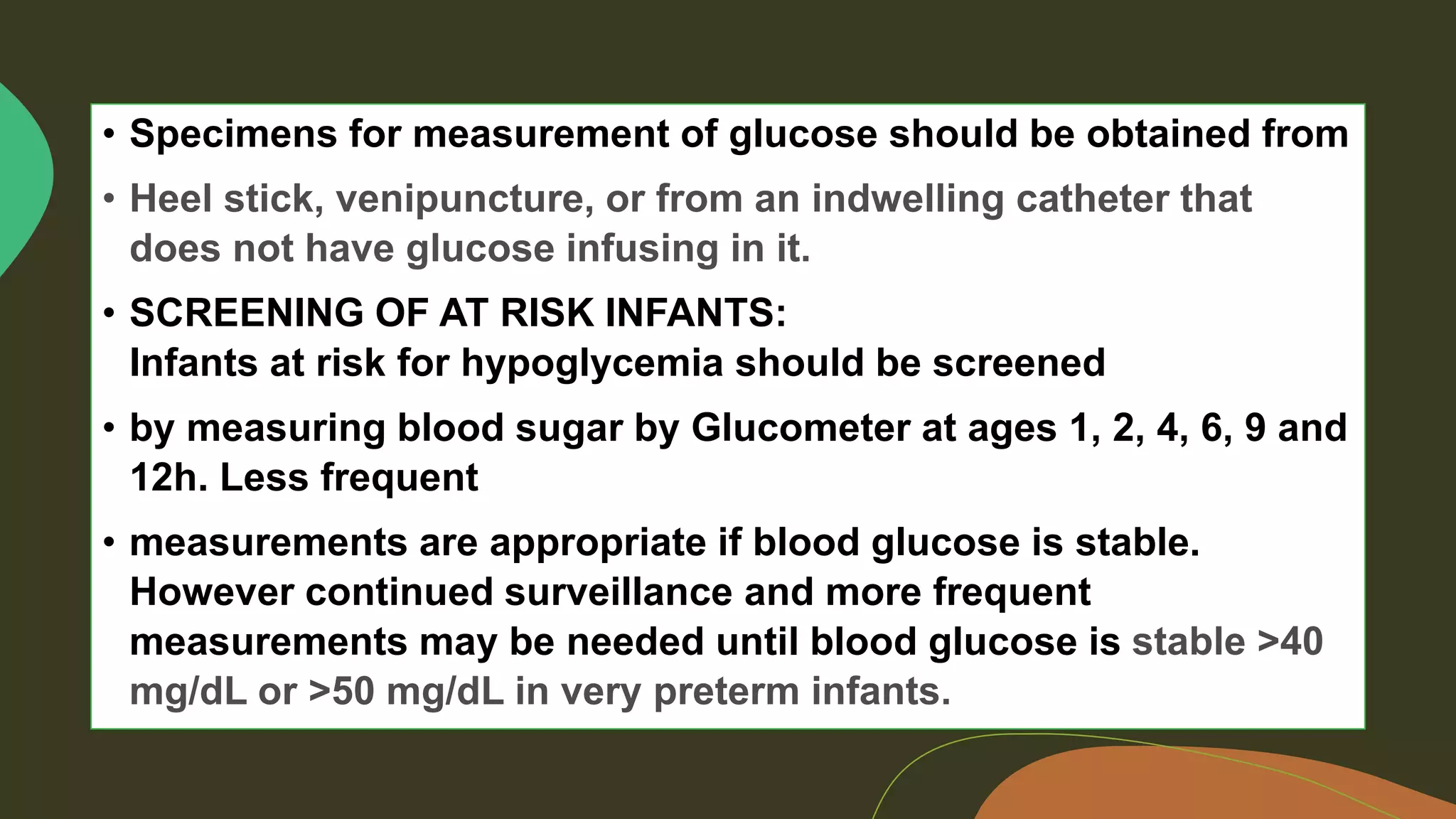
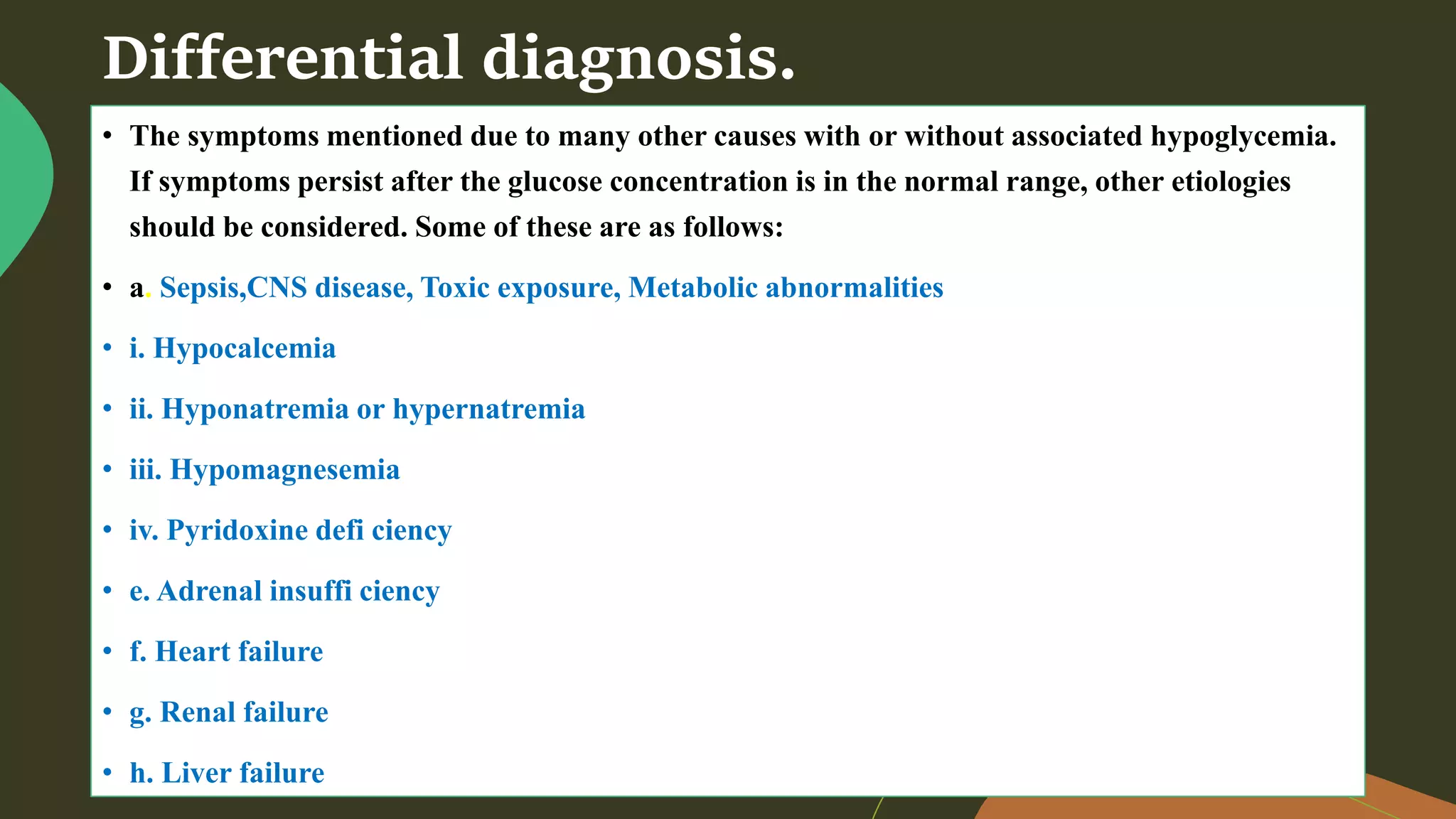
Neonatal hypoglycemia occurs when blood glucose levels drop dangerously low in newborns. It affects 5-15% of infants and can cause neurological damage if untreated. The document discusses the causes, signs, classifications, diagnosis, treatment and prevention of neonatal hypoglycemia. It emphasizes the importance of monitoring blood glucose levels in at-risk infants, providing IV dextrose or feeding to raise glucose, and supporting breastfeeding to help prevent hypoglycemia. Nursing care focuses on stabilizing blood glucose through nutrition and medical management.



























![Nursing care management
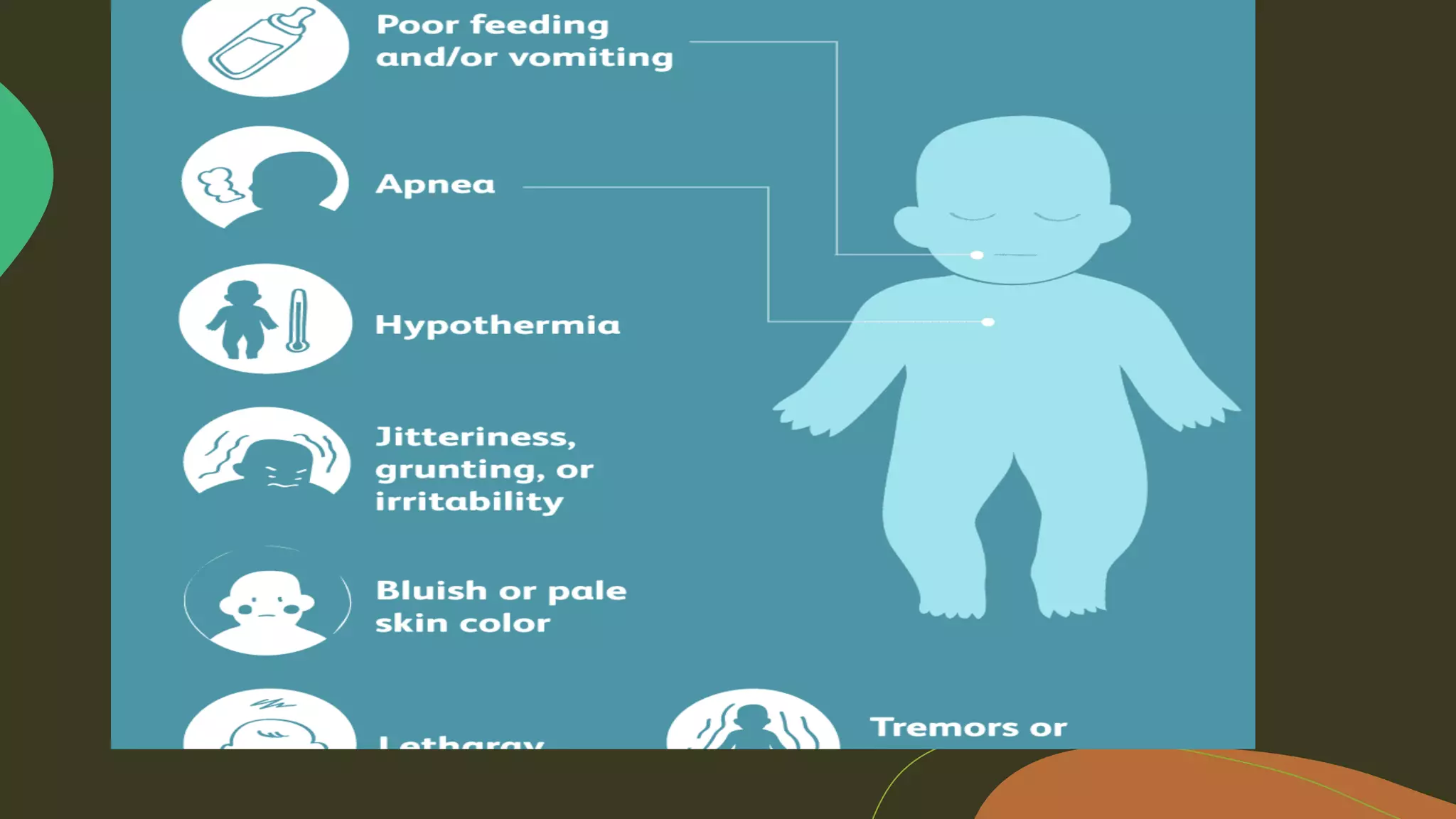
• The biggest nursing concern for a neonate experiencing hypoglycemia is the physical assessment to potentially find
the cause.[1] It is also essential to prevent environmental factors such as cold stress that may predispose the newborn
for further decreasing blood sugar.[1] Within the physical assessment, comorbidities of hypoglycemia should also be
assessed such as intolerance of feeding, or respiratory distress.[1] Another important nursing intervention is assisting
the mother in successful breastfeeding as this can prevent and treat hypoglycemia.[1]
• If an IV infusion of 10% dextrose in water is initiated then the nurse must monitor for:
• •Circulatory overload[1]
• •Hyperglycemia[1]
• •Glycosuria[1]
• •Intracellular dehydration[1]](https://image.slidesharecdn.com/managementofneonatalhypoglycemiappt-210310175346/75/Management-of-neonatal-hypoglycemia-ppt-47-2048.jpg)



