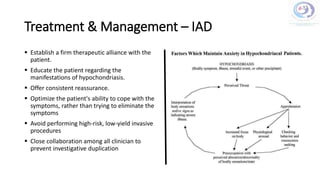
The document discusses illness anxiety disorder (IAD), outlining a case study of a 45-year-old male engineer who is preoccupied with having cancer despite inconclusive medical evaluations. It highlights the challenges in diagnosing and treating IAD, emphasizing its psychological complexities and the importance of a collaborative treatment approach involving various healthcare professionals. The document also reviews epidemiology, symptoms, causes, and several treatment strategies, including cognitive-behavioral therapy and pharmacotherapy.