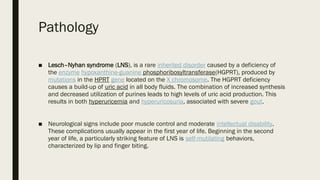
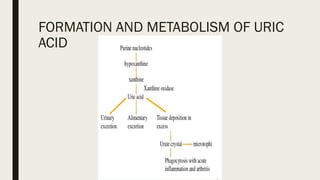
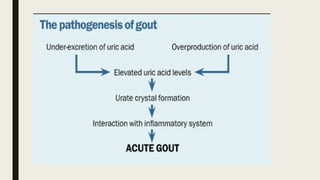
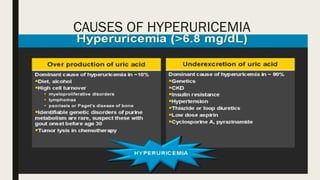
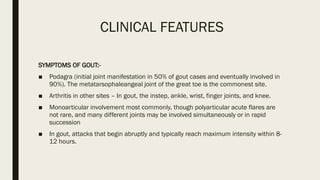
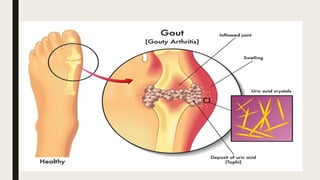
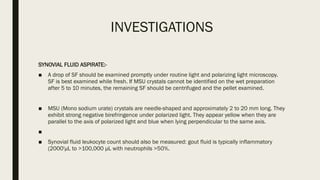
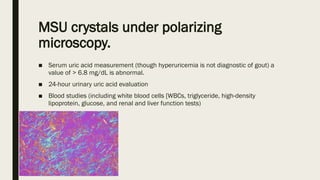
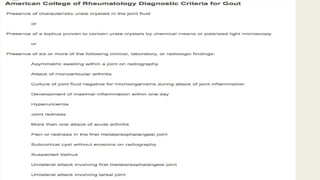
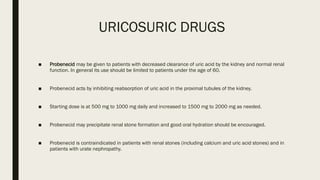
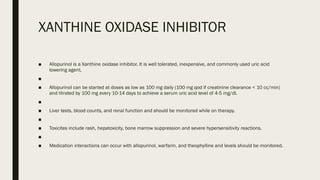
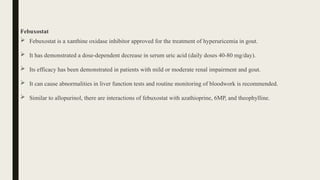
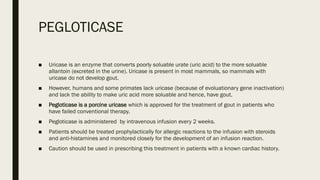
The document provides a comprehensive overview of acute gout, detailing its aetiology, clinical features, investigations, and treatment options. It highlights the role of uric acid in gout pathogenesis, common joint symptoms, complications, diagnostic investigations, and various treatment methodologies including NSAIDs, colchicine, corticosteroids, uricosuric drugs, and xanthine oxidase inhibitors. The document emphasizes the importance of addressing both acute flares and long-term management to prevent recurrence and complications.