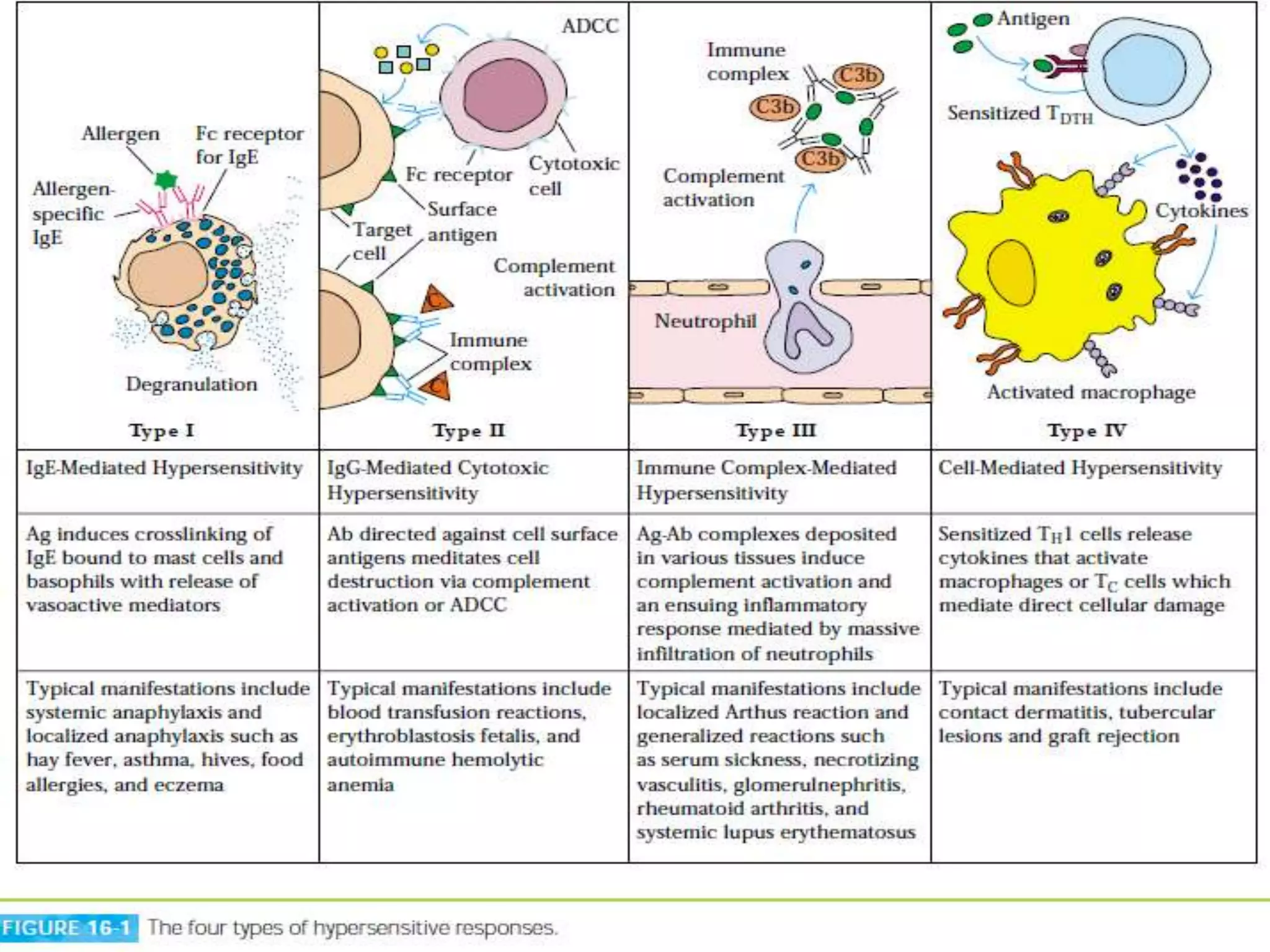
This document discusses types I and II hypersensitivity reactions. It begins by defining hypersensitivity reactions as exaggerated or inappropriate immune responses against antigens or allergens. It then discusses the classification system proposed by Gell and Coombs which divides hypersensitivity into four types: IgE-mediated (type I), antibody-mediated/IgG-mediated cytotoxic (type II), immune complex-mediated (type III), and cell-mediated or delayed-type hypersensitivity (type IV). The document focuses on types I and II, providing details on the mechanisms, examples, and treatments of IgE-mediated and antibody-mediated cytotoxic hypersensitivity reactions.