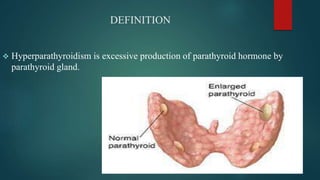
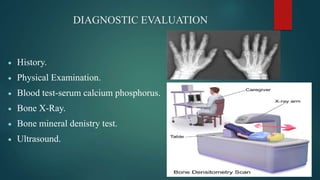
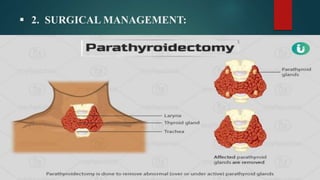
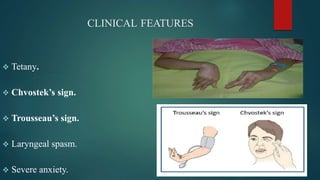
This document discusses hyperparathyroidism and hypoparathyroidism. Hyperparathyroidism is defined as excessive production of parathyroid hormone and can be primary, secondary, or tertiary. It causes increased calcium levels and symptoms include kidney stones and bone problems. Hypoparathyroidism is insufficient parathyroid hormone leading to low calcium and high phosphorus levels, and can result from surgery or genetic factors. It causes low calcium symptoms like tetany. Both conditions involve abnormal parathyroid hormone levels impacting calcium regulation.