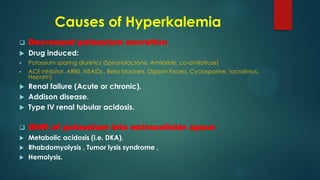
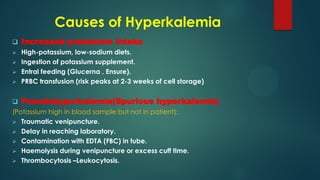
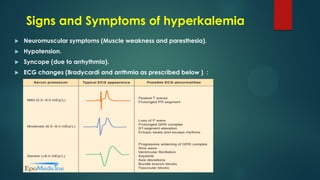
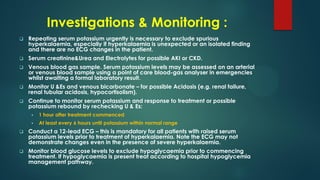
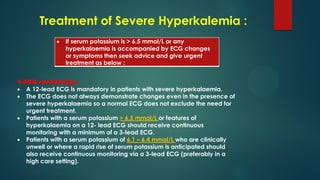
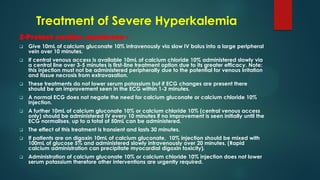
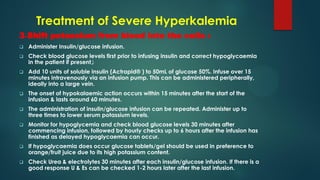
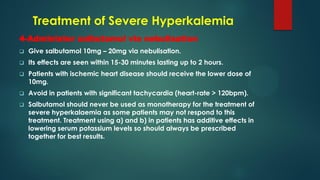
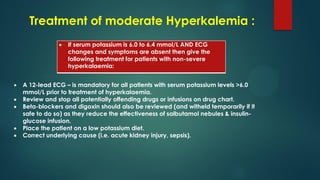
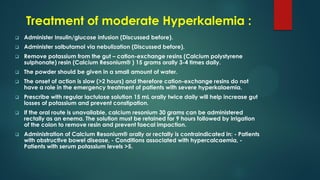
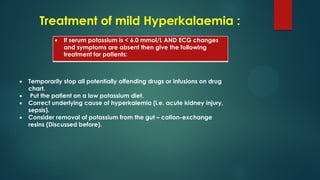
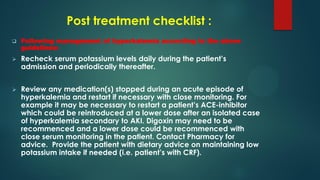
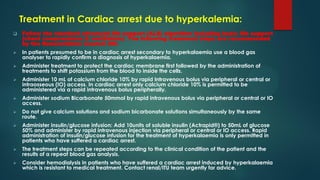
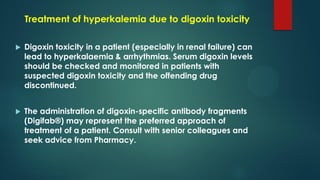
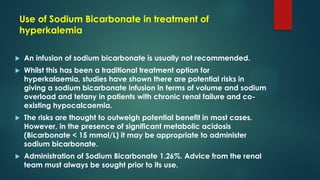
This document provides guidelines for the management of hyperkalemia according to NICE guidelines. It defines mild, moderate and severe hyperkalemia based on potassium levels. It describes the causes, signs and symptoms, and appropriate investigations. For severe hyperkalemia when potassium is >6.5 mmol/L or ECG changes are present, the guidelines recommend ECG monitoring, protecting the cardiac membrane with calcium, shifting potassium into cells with insulin/glucose, administering salbutamol via nebulization, stopping further potassium accumulation and considering hemodialysis if levels remain high. For moderate hyperkalemia when potassium is 6.0-6.4 mmol/L and no ECG changes, the guidelines recommend insulin/