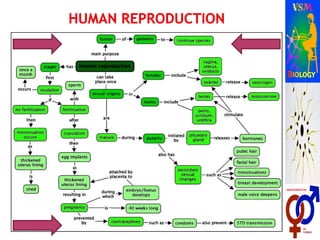
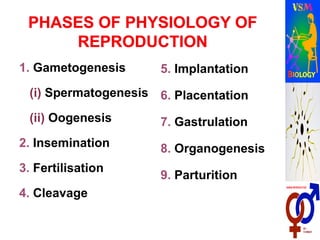
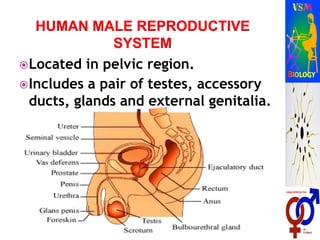
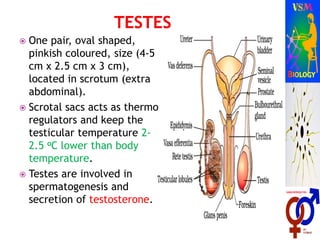
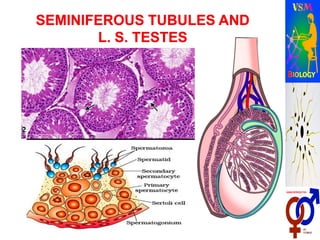
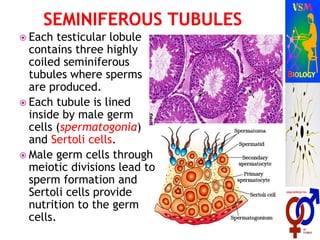
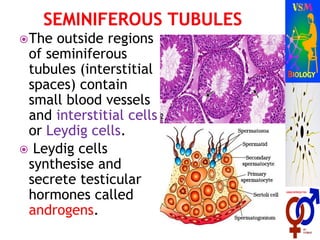
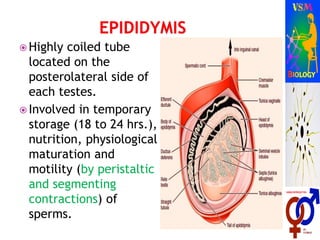
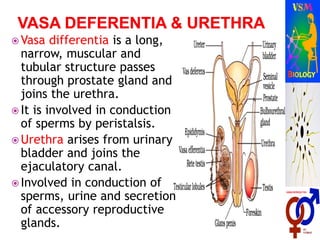
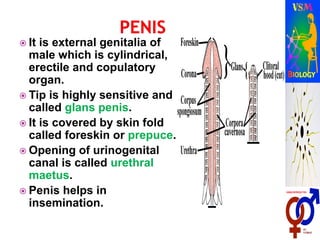
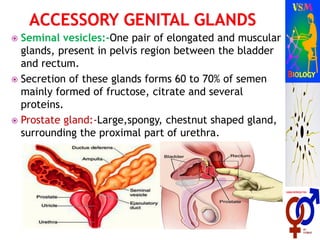
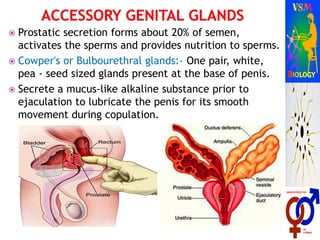
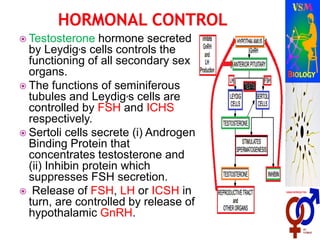
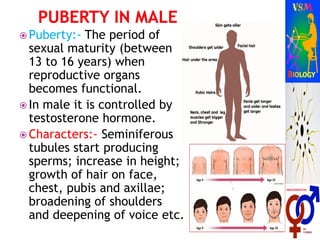
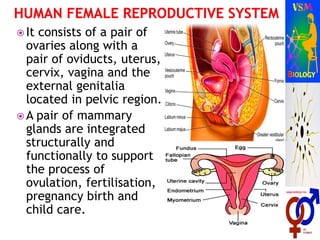
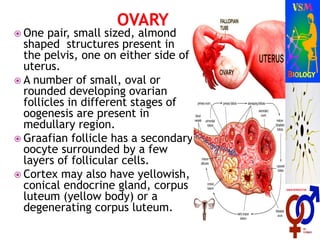
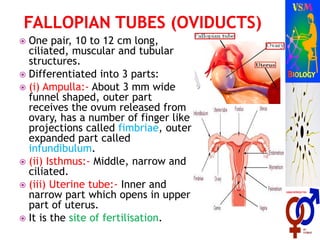
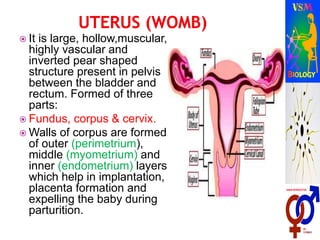
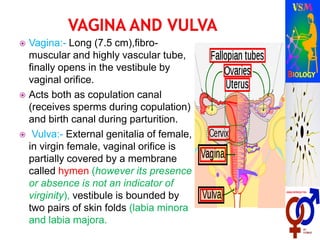
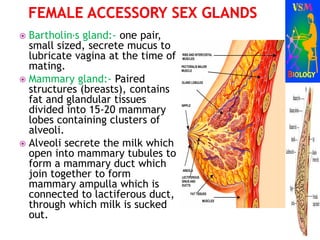
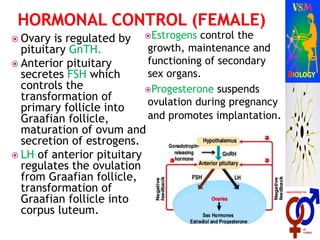
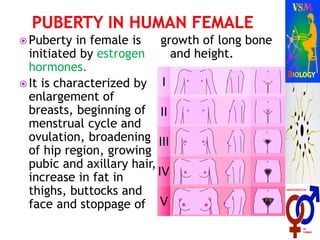
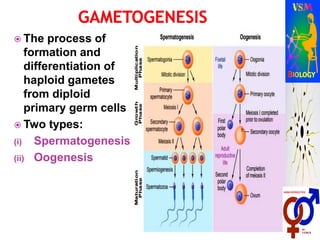
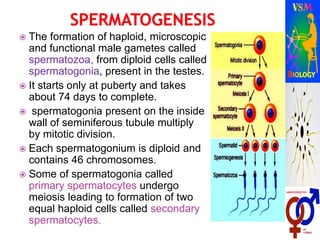
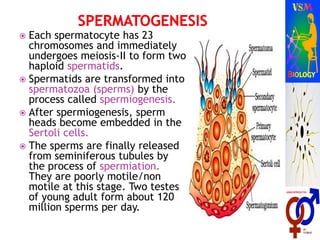
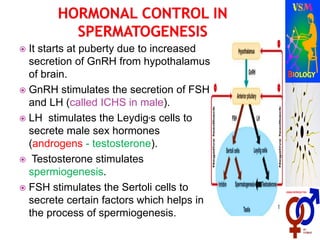
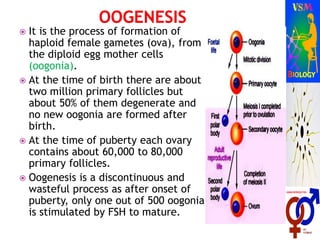
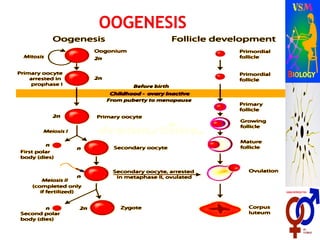
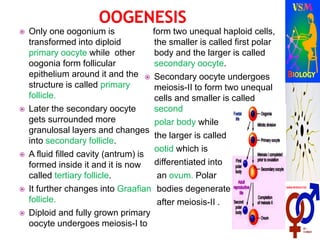
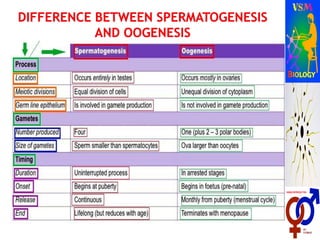
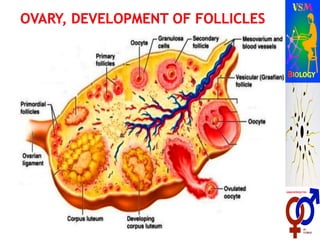
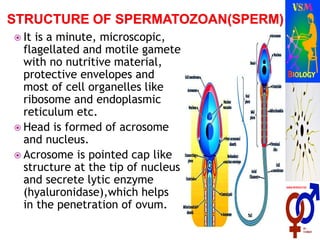
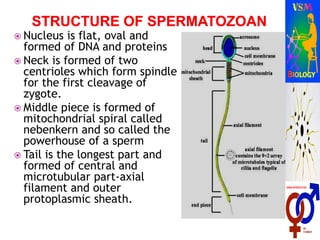
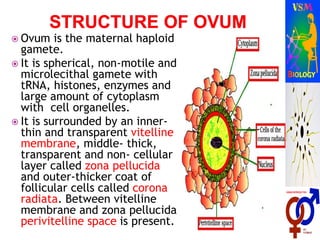
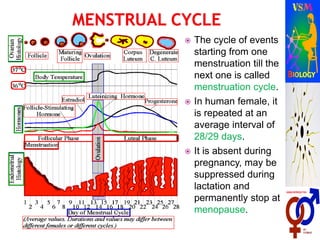
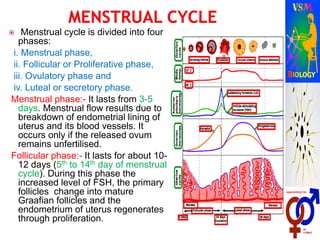
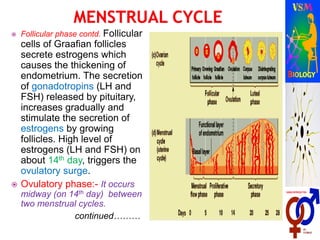
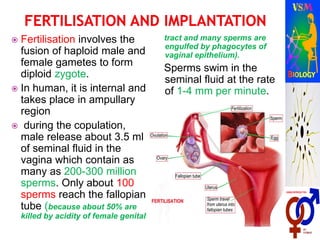
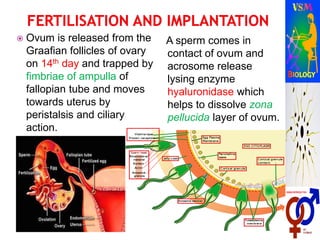
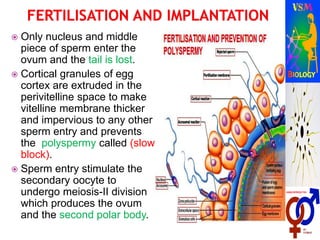
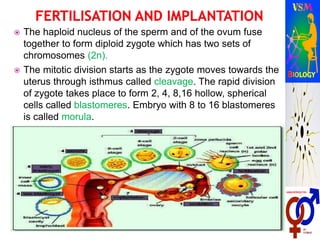
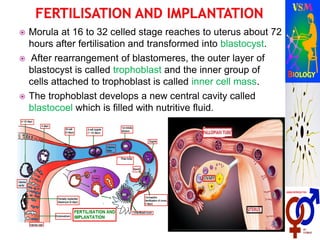
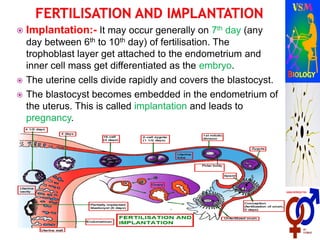
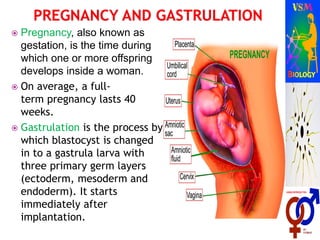
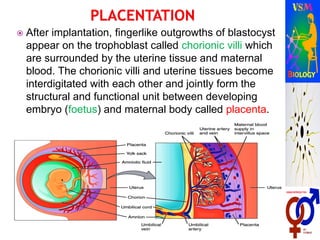
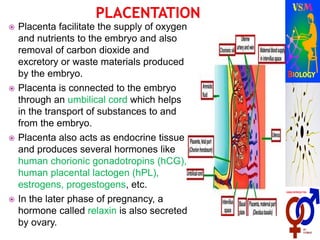
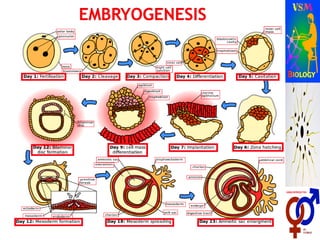
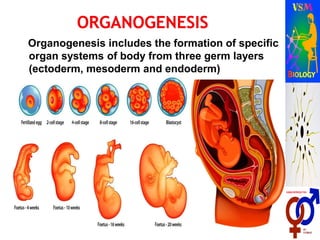
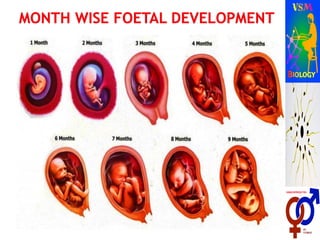
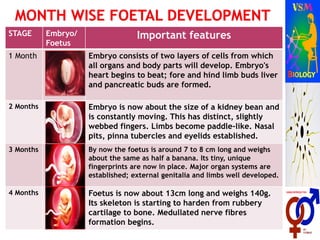
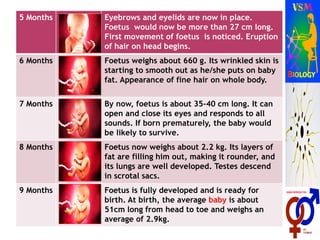
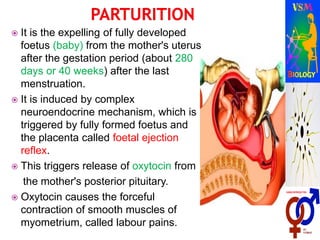
The document describes human reproductive systems and processes. It discusses that humans are viviparous and have two distinct sexes. It then describes the male reproductive system in detail, including internal structures like testes, ducts and glands, and external structures like penis. Key processes in the male like spermatogenesis and roles of hormones are explained. Similarly, the female reproductive system and structures like ovaries, uterus and mammary glands are outlined. Oogenesis and roles of hormones in female are also covered. The stages of human reproduction from fertilization to birth are briefly listed.