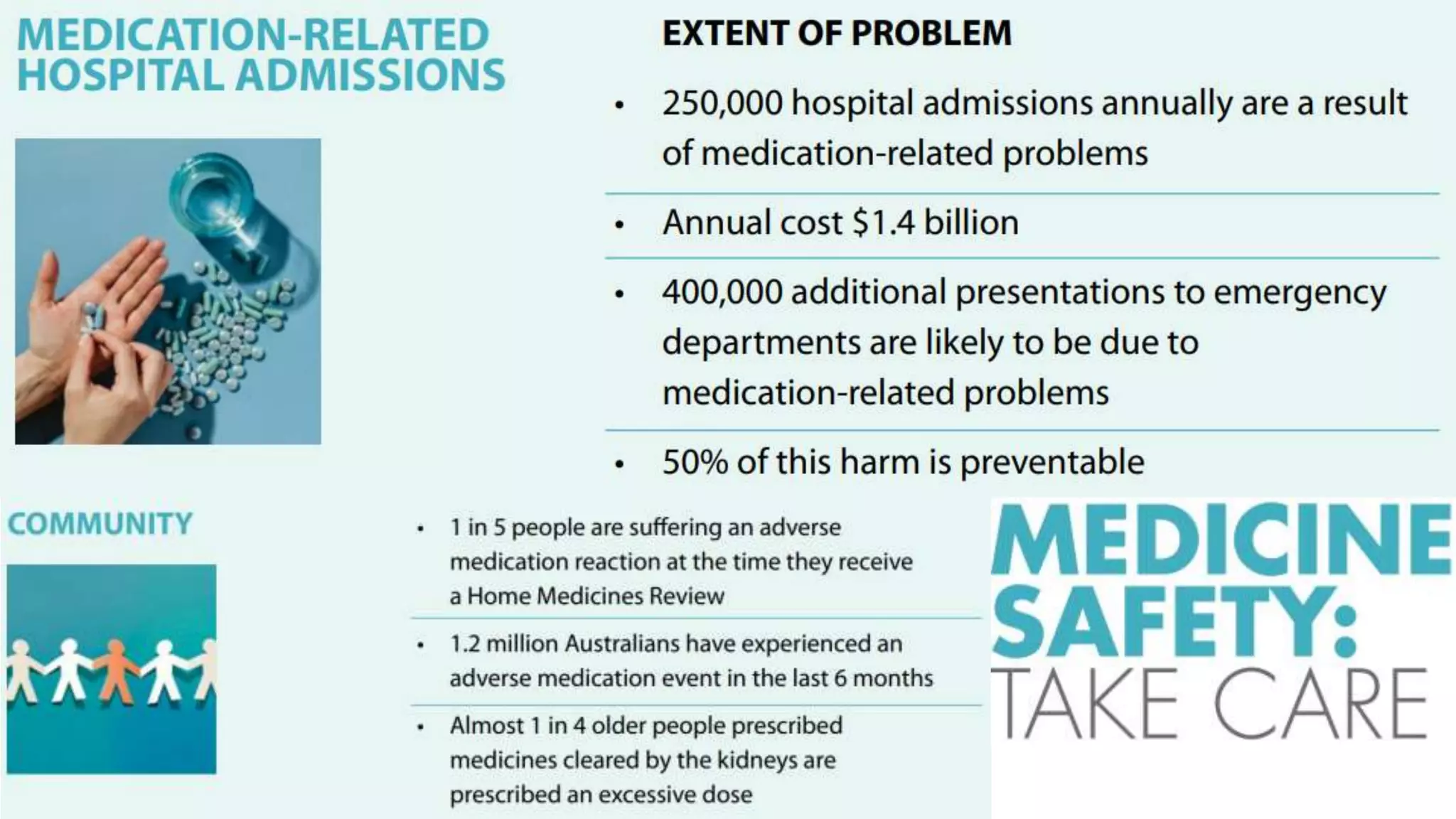
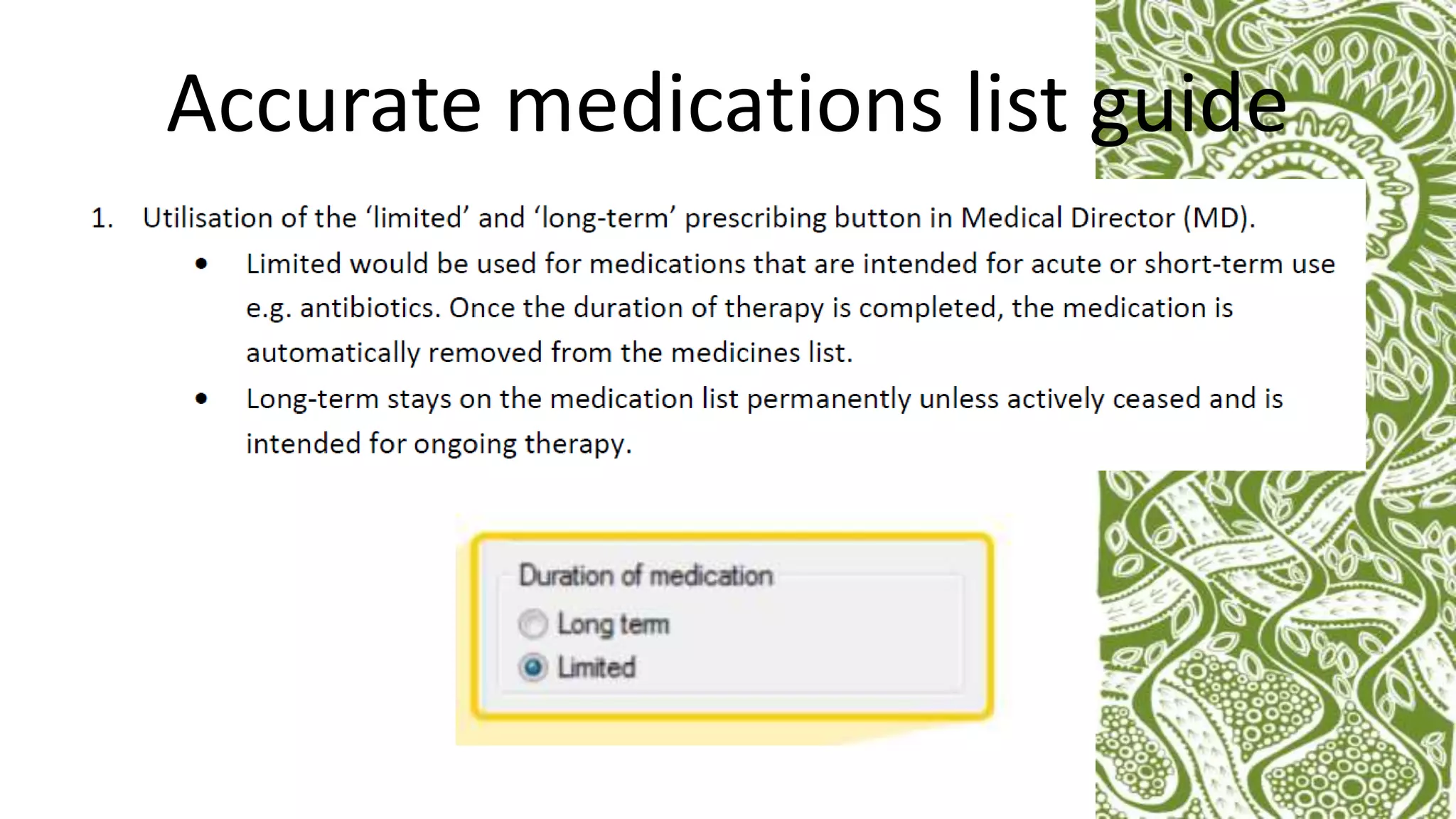
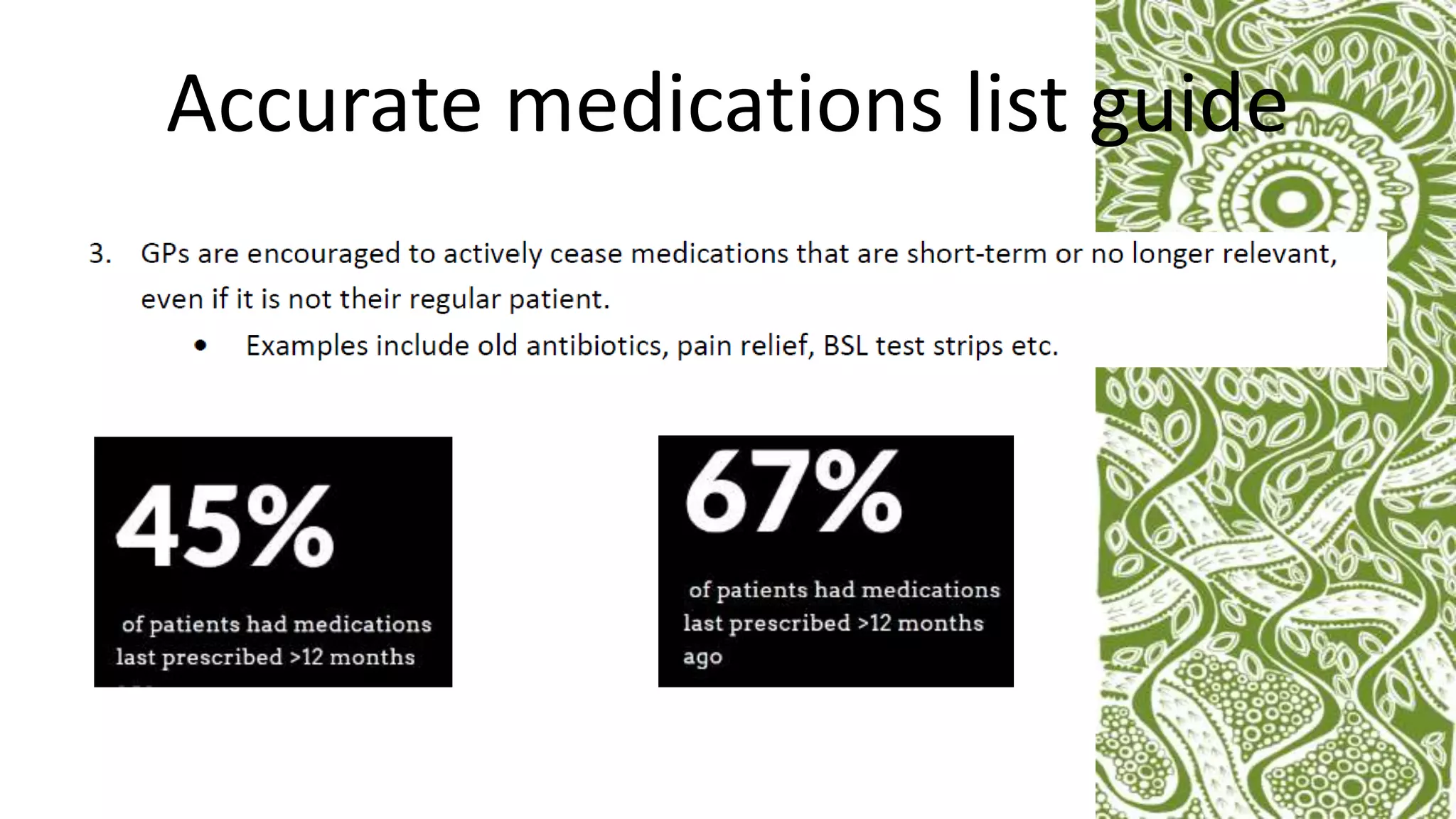
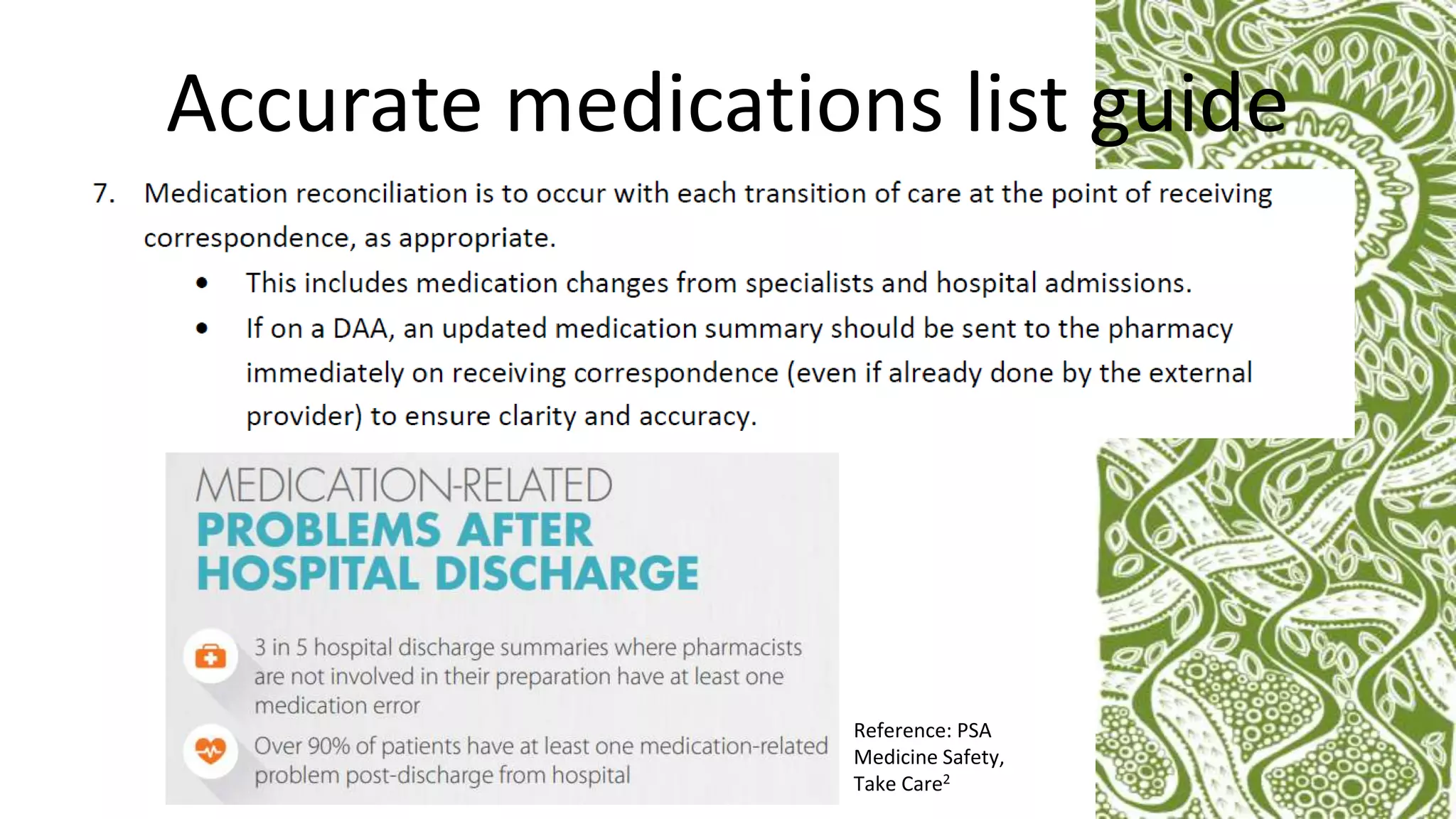
This document discusses how to keep an accurate medicines list through an organizational approach. It describes Galambila Aboriginal Health Service, which aims to ensure patients and providers receive accurate medicines lists. Regular audits of medicines lists provide a platform for sustainable change to improve accuracy. Having GP champions and understanding clinical software helps facilitate keeping accurate lists, which benefits patients, the health service, and community pharmacies. Measurable improvements will be developed through the audit process.