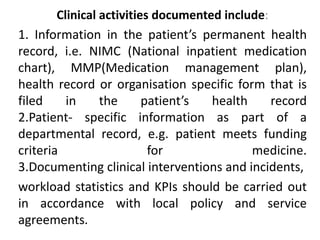
The document discusses documenting clinical pharmacy services. It states that documenting activities is essential for providing services and involves recording patient information, interventions, workload statistics, and quality indicators. The objectives of documentation are to improve patient care, communicate with other providers, demonstrate pharmacist accountability and assess service quality. Clinical activities that should be documented include information in health records, departments records, interventions, and workload/performance indicators.