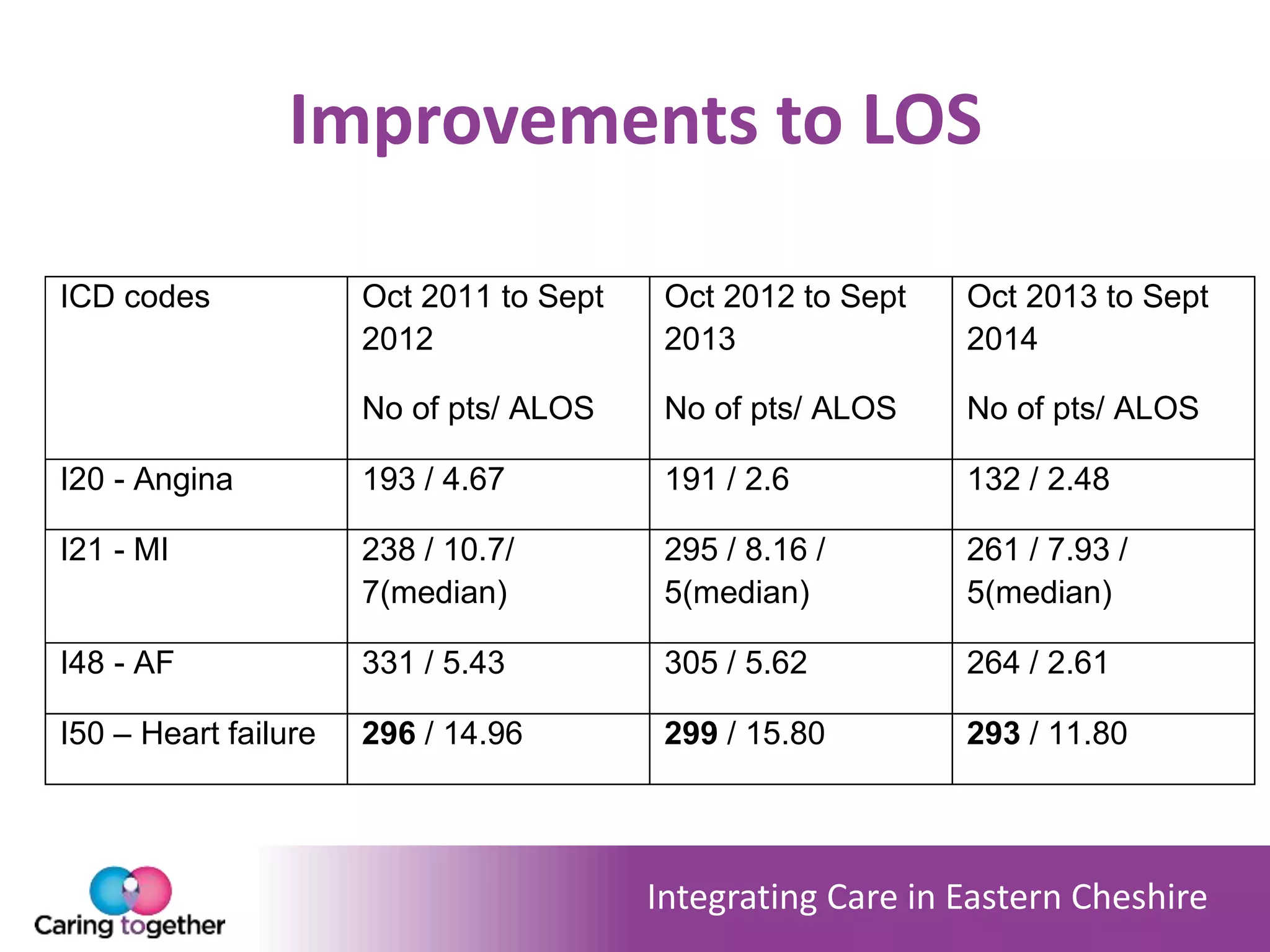
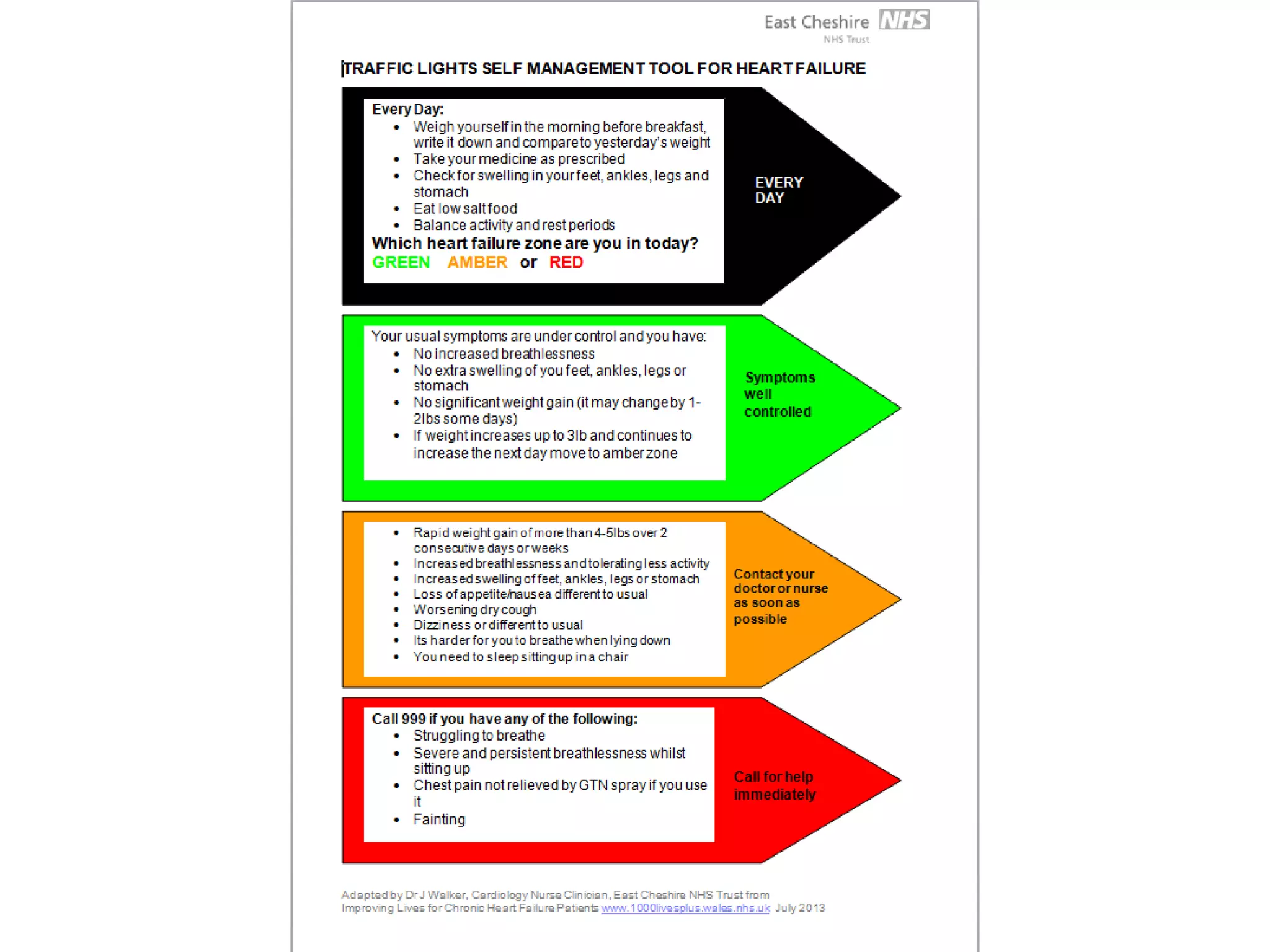
The document outlines the integration of community-based IV diuretics for advanced heart failure patients in East Cheshire, aimed at reducing hospital admissions and enhancing patient management. A successful bid led to the establishment of an integrated cardiology nurse team, facilitating at-home care and promoting self-management. Positive outcomes include stable heart failure admissions and significant cost savings, while ongoing challenges have been addressed to improve service delivery.