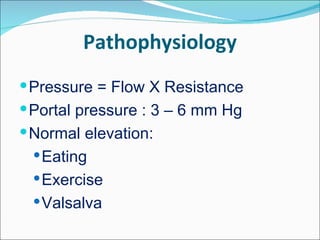
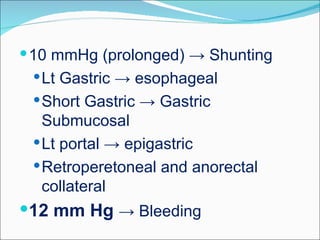
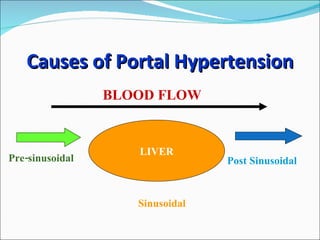
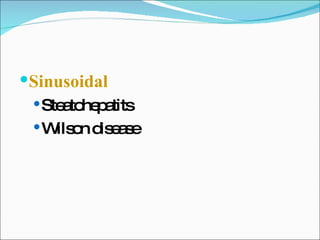
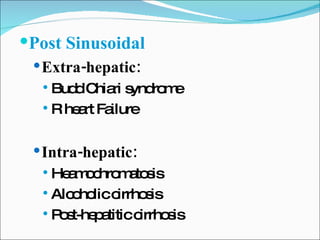
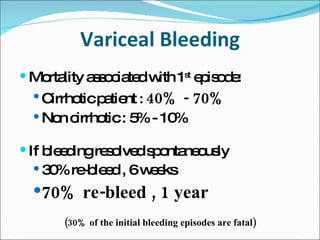
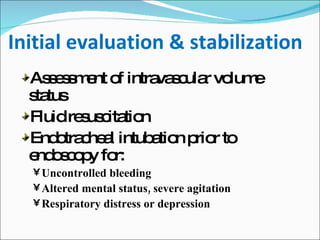
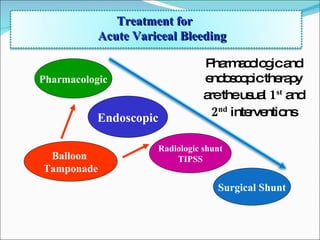
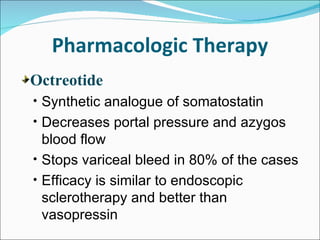
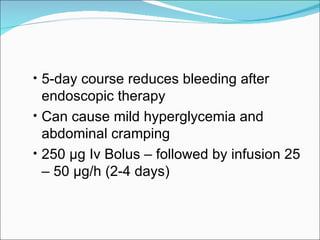
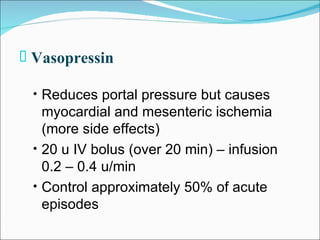
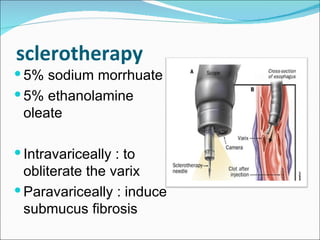
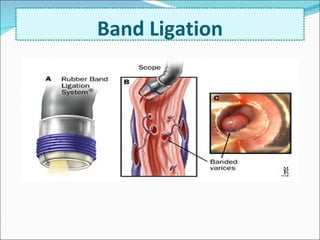
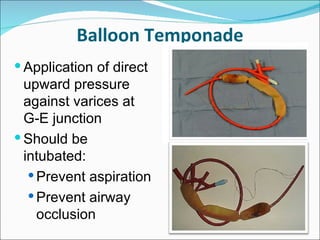
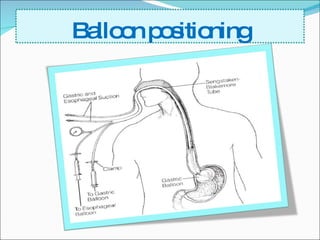
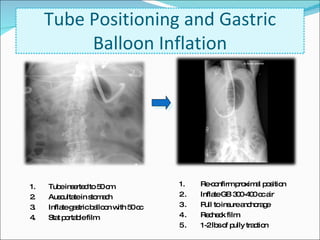
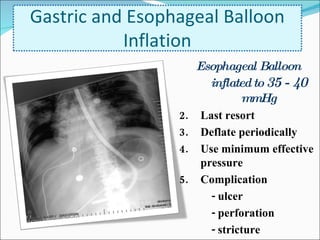
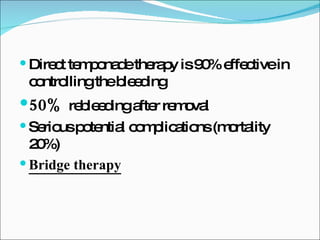
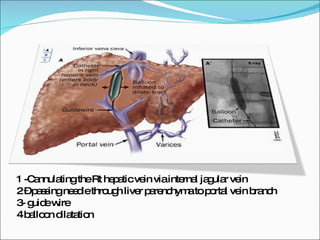
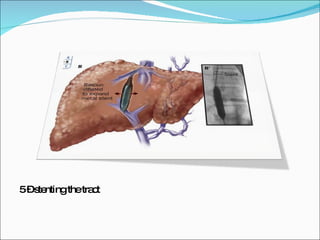
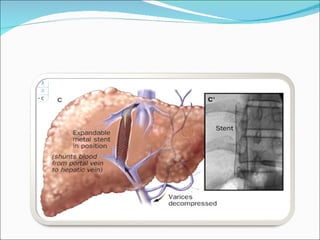
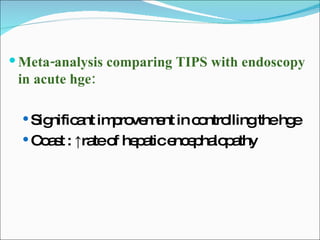
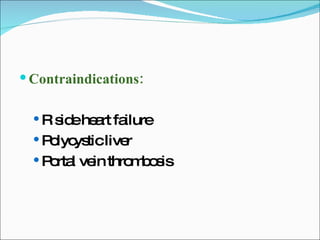
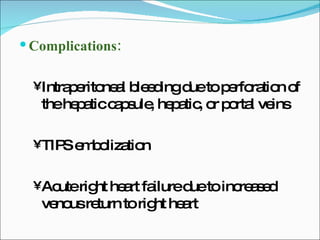
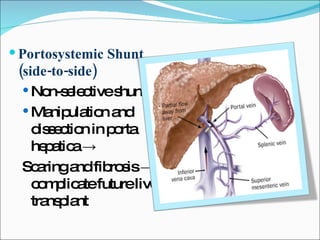
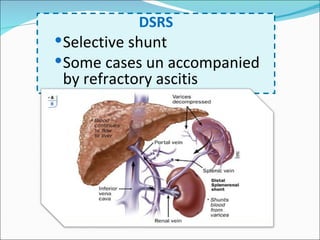
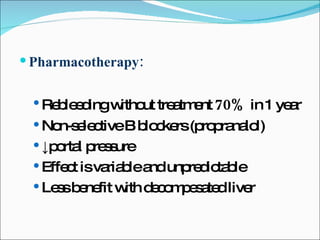
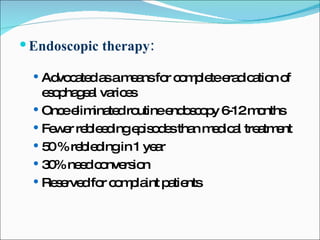
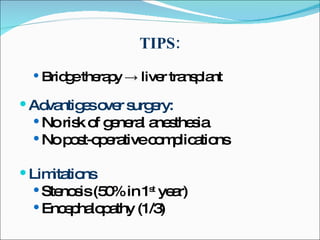
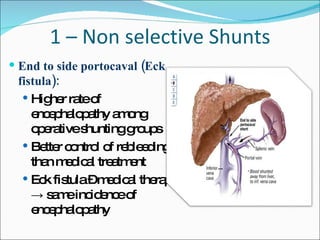
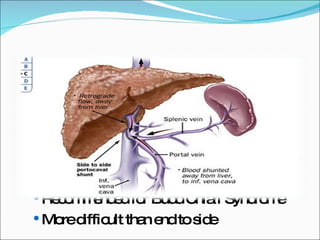
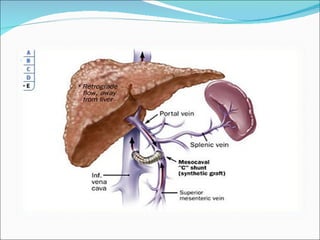
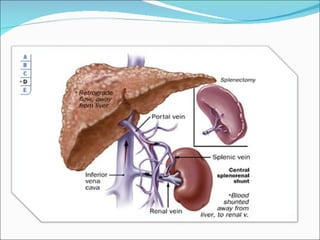
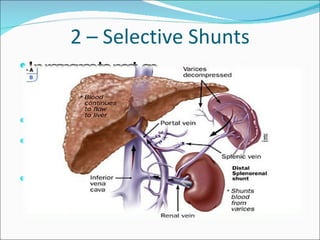
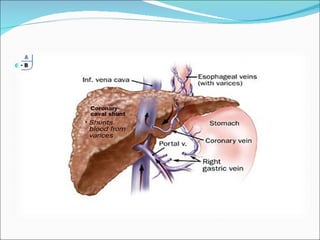
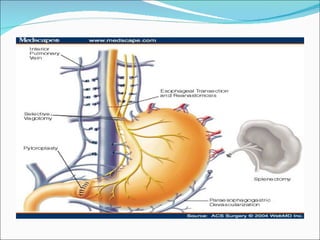
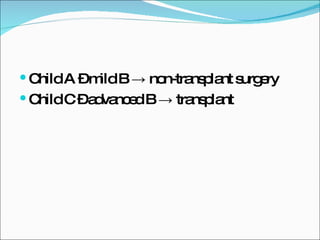
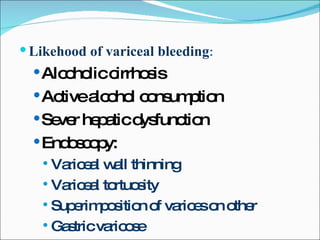
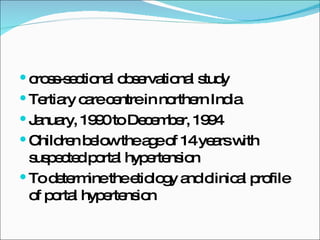
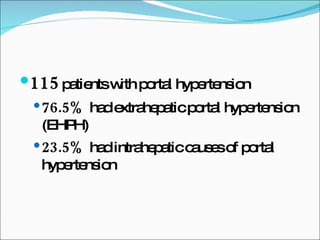
This document summarizes information about portal hypertension and variceal bleeding. It discusses the causes of portal hypertension including pre-sinusoidal, sinusoidal and post-sinusoidal factors. It also describes treatments for acute variceal bleeding such as pharmacologic therapies, endoscopic therapies like band ligation, balloon tamponade and TIPS. It notes that prevention of recurrent bleeding involves pharmacotherapy, endoscopic therapy, TIPS or surgical options like portosystemic shunts or liver transplantation.