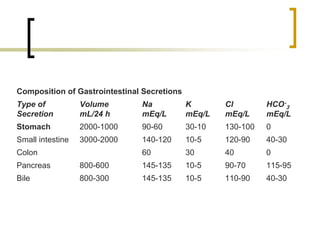
1) Fluid and electrolyte management is paramount for surgical patients as changes can occur pre, intra, and post operatively due to various factors.
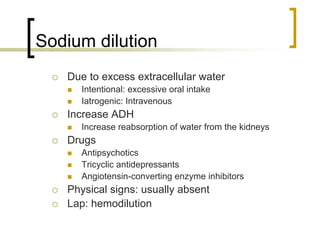
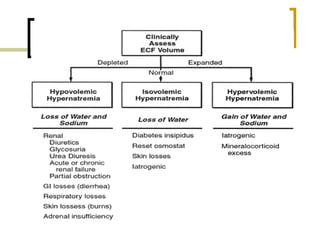
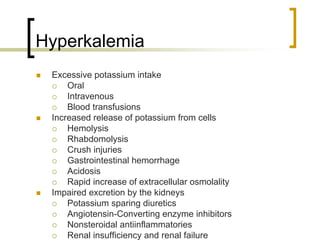
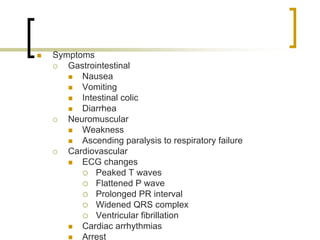
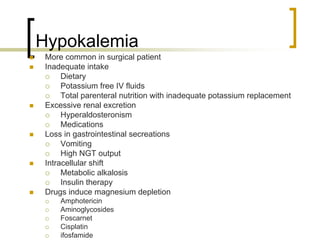
2) Sodium and potassium disturbances are common and can cause issues in multiple body systems if not properly managed.
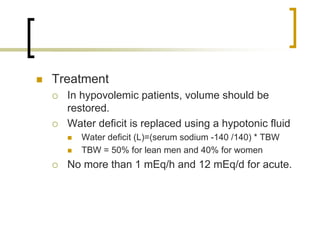
3) Treatment for abnormalities involves identifying the cause, restoring fluid and electrolyte deficits or excesses slowly and carefully based on symptoms and monitoring to prevent further complications.