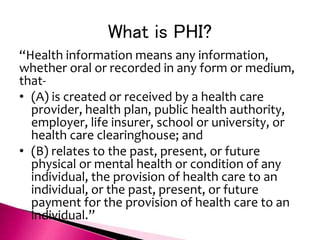
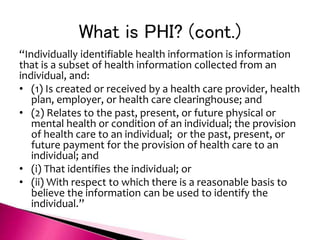
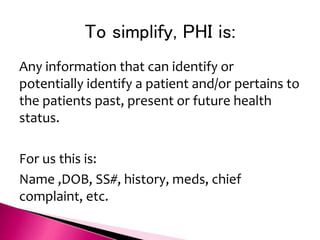
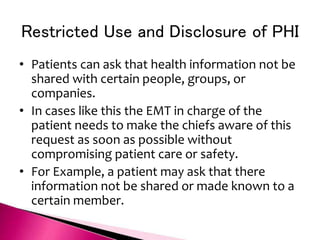
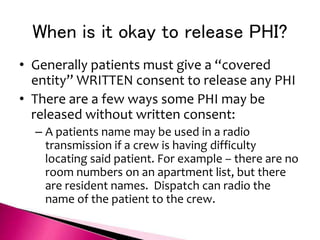
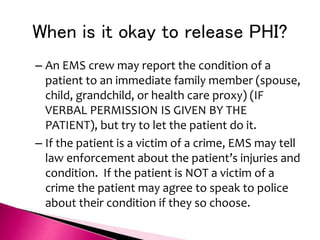
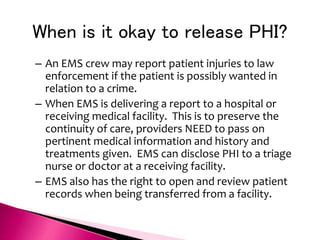
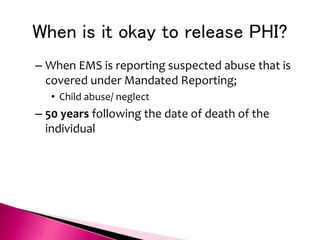
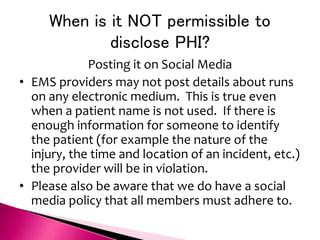
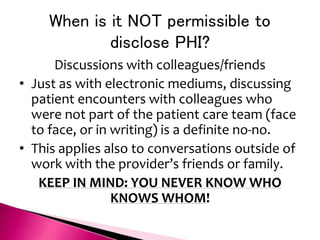
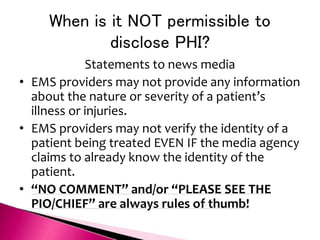
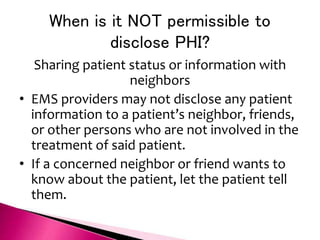
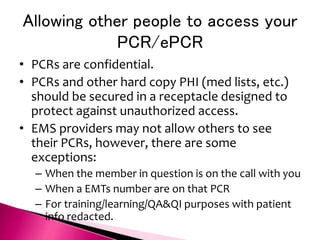
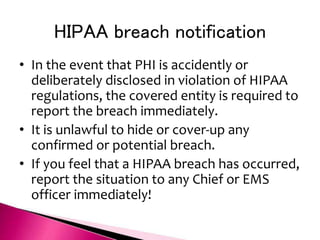
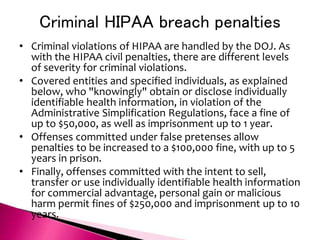
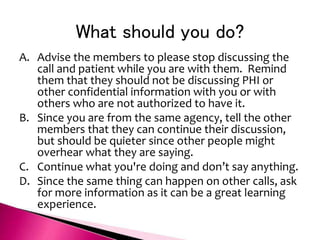
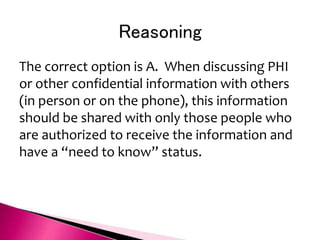
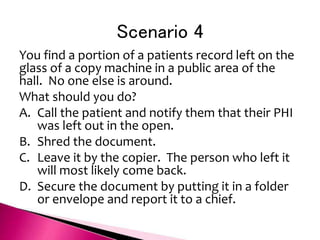
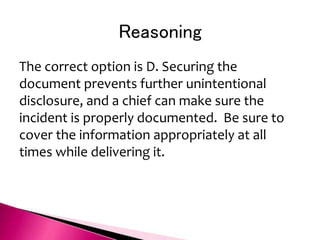
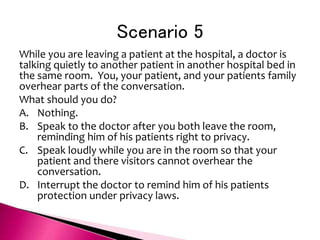
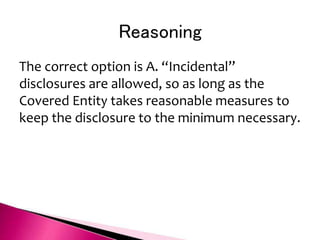
The document discusses HIPAA regulations regarding protected health information (PHI). It defines PHI and explains that HIPAA aims to protect patient privacy. It outlines who is considered a Covered Entity bound by HIPAA and provides examples of when PHI can and cannot be disclosed. Specific rules are given around securing, sharing, and disposing of PHI to prevent violations.