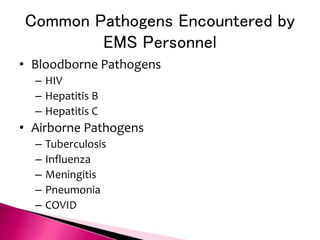
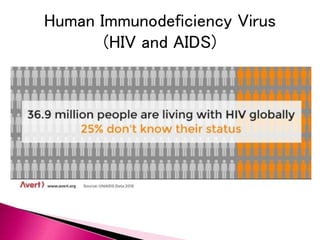
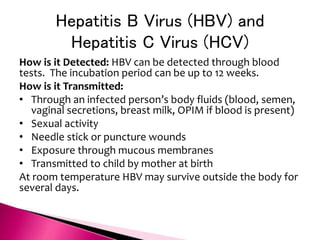
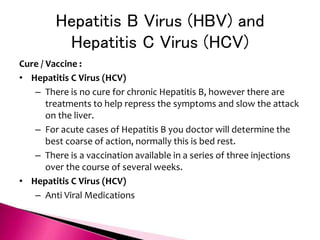
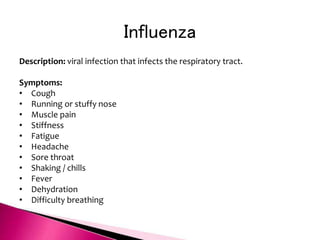
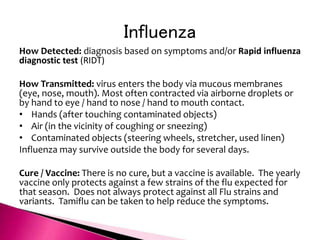
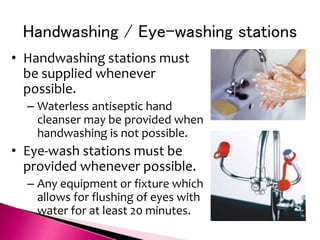
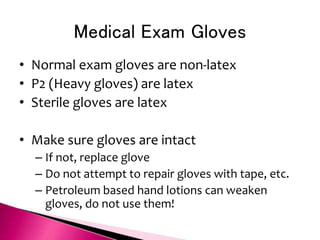
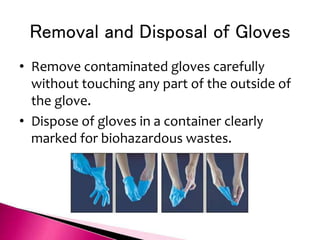
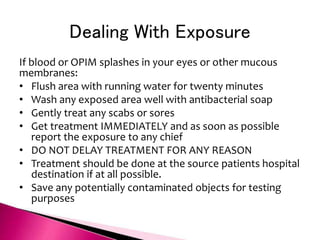
The document discusses OSHA's Bloodborne Pathogen Standard which requires annual training for employees exposed to blood and other potentially infectious materials. It covers who is covered under the standard, potential pathogens, how pathogens are transmitted, and common precautions to prevent exposure such as use of personal protective equipment, proper handling of sharps and regulated waste, decontamination procedures, and universal precautions to treat all blood and body fluids as potentially infectious. It also provides guidance for immediate treatment in the event of an exposure.