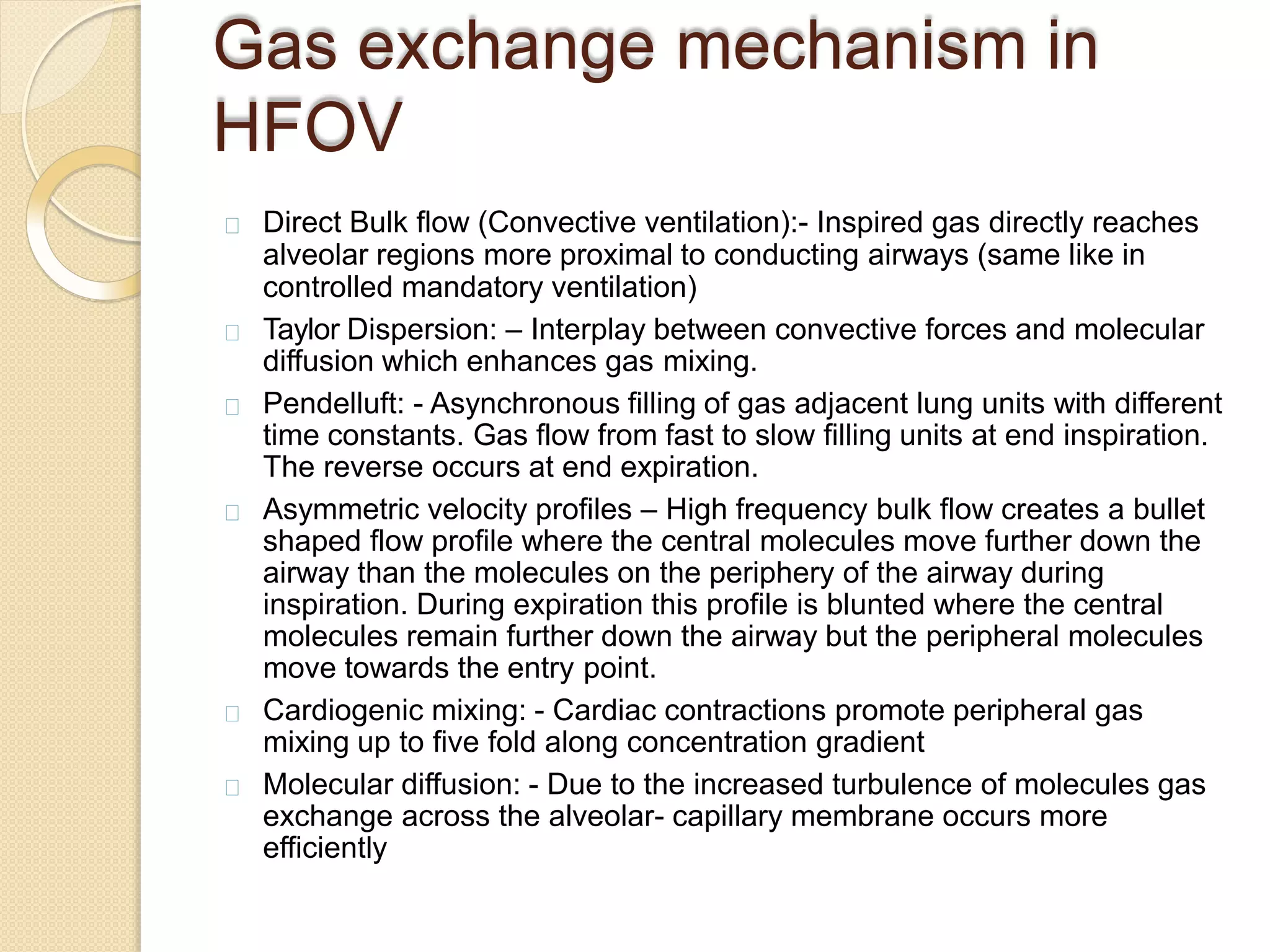
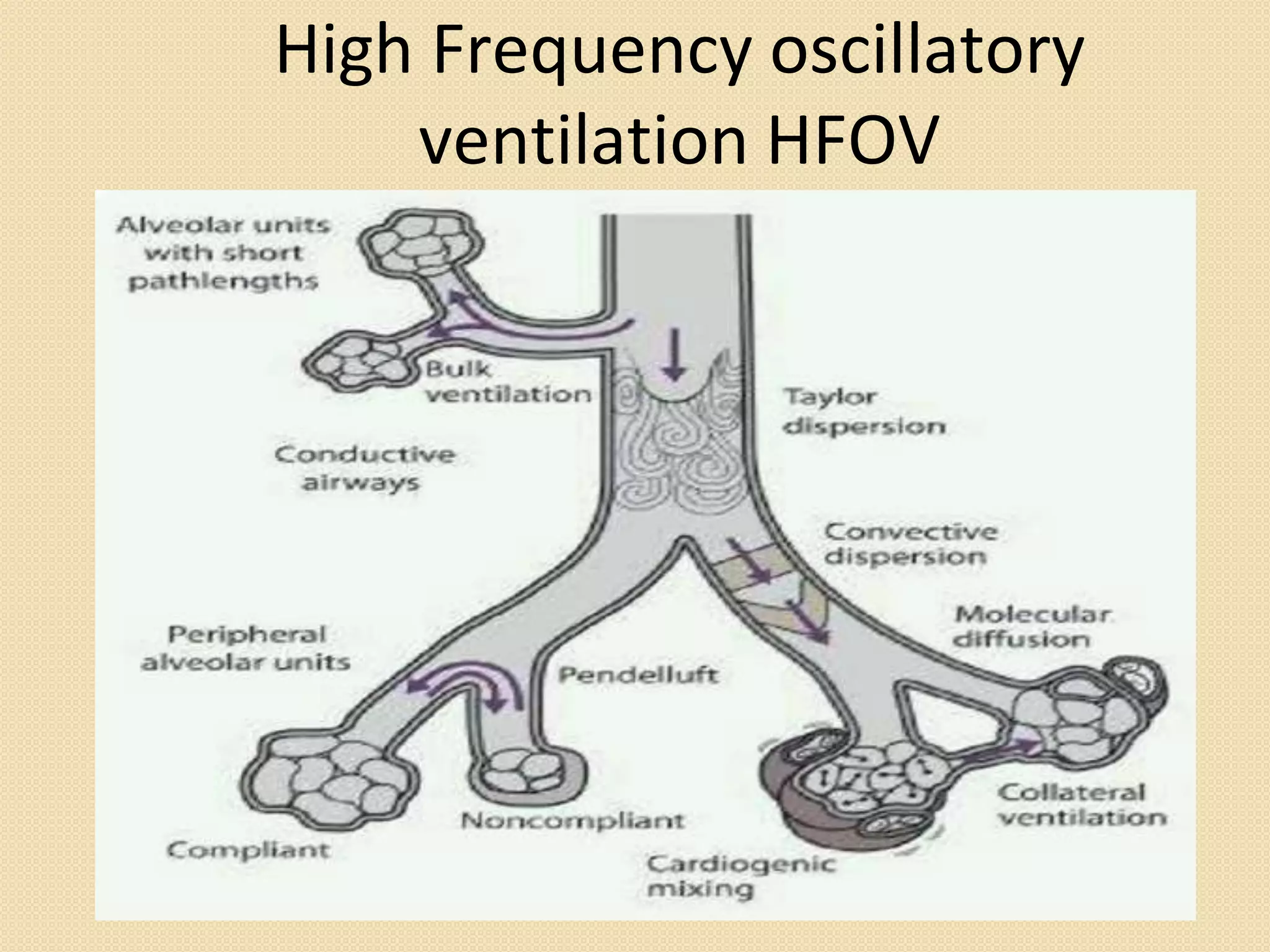
High frequency oscillatory ventilation (HFOV) delivers very small tidal volumes at high frequencies to open collapsed alveoli and improve gas exchange. It maintains constant high mean airway pressure to prevent alveolar collapse between breaths. This recruits more lung volume and improves oxygenation compared to conventional ventilation. HFOV is used as a rescue therapy when conventional ventilation fails to oxygenate patients with severe acute respiratory distress syndrome or lung injuries from burns, trauma or other causes. Potential complications include pneumothorax, hemodynamic instability and difficulties with sedation, transport and monitoring.