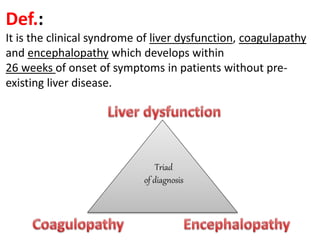
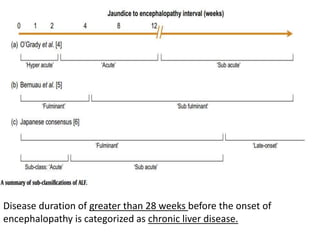
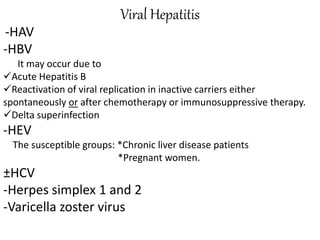
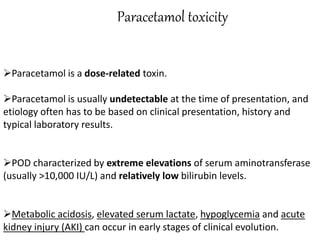
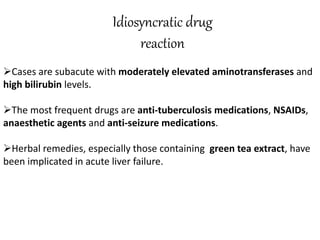
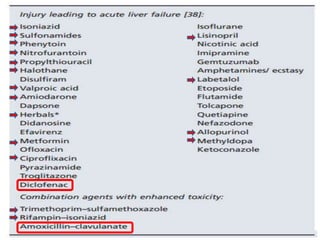
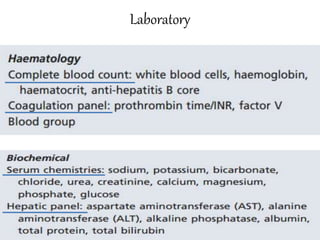
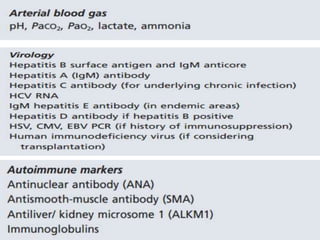
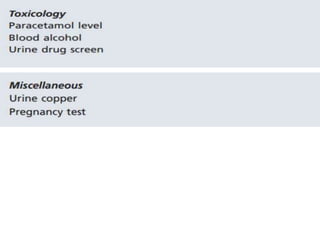
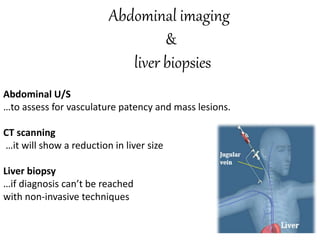
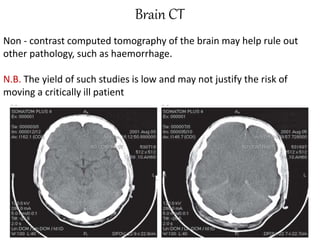
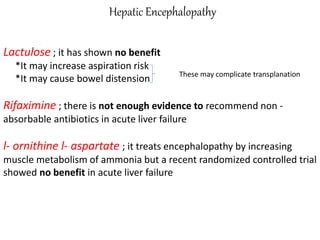
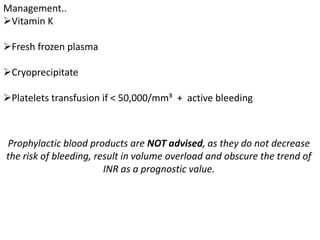
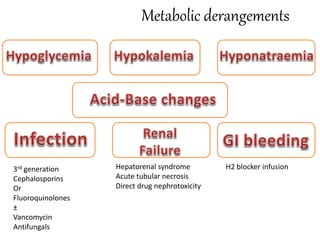
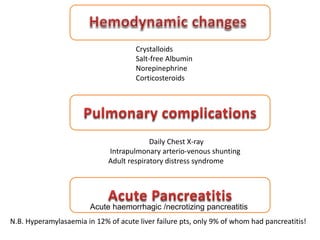
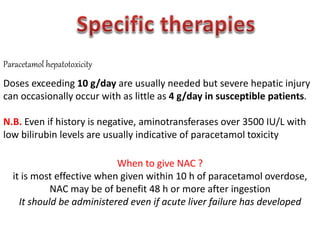
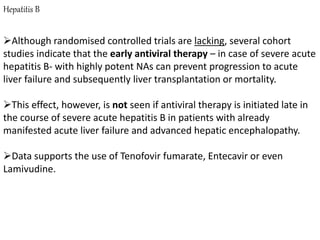
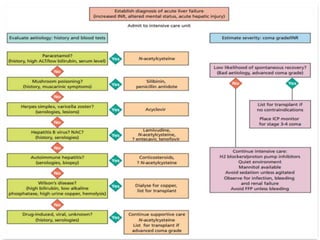
Fulminant hepatitis is a severe clinical syndrome of liver dysfunction characterized by coagulopathy and encephalopathy, developing within 26 weeks in patients without pre-existing liver disease. Key causes include viral hepatitis, drug toxicity, metabolic disorders, and vascular issues, leading to non-specific symptoms, jaundice, and complications like hepatic encephalopathy and renal failure. Management focuses on treating complications and specific causes, with liver transplantation being a critical option in severe cases.