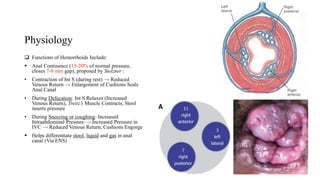
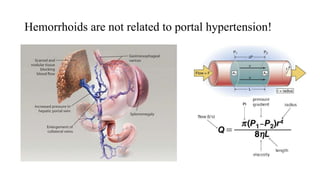
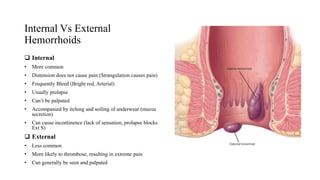
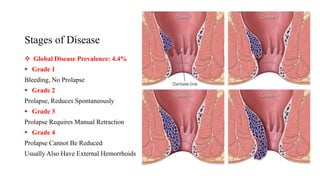
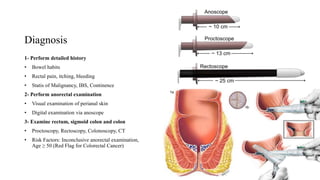
Hemorrhoids are normal anal cushions that help with continence. They become symptomatic when the veins and connective tissue deteriorate, causing swelling. Hemorrhoids are either internal or external. Internal hemorrhoids are more common and cause bleeding but not pain, while external hemorrhoids cause pain but rarely bleed. Hemorrhoids are graded based on severity from stage 1 with no prolapse to stage 4 that cannot be reduced. Treatment depends on the stage but may include lifestyle changes, creams, banding or surgery.